Digitech’s 2025 calendar keeps rolling with a robust lineup of EMS conferences in Q3. These events offer an opportunity to engage with EMS leaders, exchange ideas, and highlight how our billing solutions can help agencies thrive. Take a look at where we’ll be this quarter!
Reach Out to Our Team
Meet Digitech at EMS Industry Events – Q2 2025
Digitech continues its 2025 journey with a packed schedule of industry-leading conferences in Q2. These events are our chance to connect with EMS professionals, share expertise, and showcase how our billing solutions support agencies nationwide. Check out where we’ll be this quarter!
Reach Out to Our Team
Saving Lives for Low Wages: The Issue of Pay Equity in EMS
Careers in Emergency Medical Services can be deeply fulfilling. But staffing and retention continue to be huge problems for the industry. Why?
EMS providers are underpaid.
There are a variety of complex forces that push salaries for EMS to the bottom of the healthcare industry’s pay scales. A primary factor is the funding structure of EMS agencies. The way EMS is currently billed and funded makes the service free to community members… until they actually need the service. As healthcare has become more expensive overall, both public and private payers have reduced what they are willing to pay for these services. This squeeze on revenues leads to an inevitable need to reduce personnel expenses, which are the largest component of EMS budgets[1].
Another contributor to the low pay of EMS providers is the resistance to formal education within the profession. This resistance can negatively affect prevailing wages[1]. The certification required to become an EMT or paramedic is relatively minimal, which can also contribute to lower wages. It only takes 120 to 150 hours of training to become an EMT, and ambulances in rural communities are often staffed by volunteers, which depresses wages for those who do pursue the role as a career[2].
Discrimination also plays a role in keeping wages low. For instance, in New York City, EMS workers have claimed that gender and racial discrimination keep their wages low and their prospects for advancement limited, making them “third-class citizens.”[3] The workforce of EMS in New York City is predominantly women and minorities. On the other hand, the FDNY (of which EMS is a division) has a predominantly white leadership. According to City data, FDNY EMS is 59% non-white, 89% male, and 12% female but women and minorities make up only 11% of the FDNY EMS workforce at the rank of Deputy Chief and above (2019 data).”[4] While these trends may not directly dictate low wages across the entire industry, the effect of discrimination reverberates throughout staffing and retention. If you may get stuck in a low-paying role, why start in the first place?
The pay structure for EMS workers is also influenced by the perceived nature of the work, which is often viewed as less high-risk and stressful than other public safety jobs. The rising number of attacks on EMS personnel indicates otherwise. According to the U.S. Centers for Disease Control and Prevention, 2,000 EMS professionals are injured every year in violence-related incidents. Despite the dangers, EMS workers are often paid less than other first responders like firefighters and police officers[5]. Again, using NYC as an example, the starting pay for a FDNY EMS EMT is just $35,000, a wage difficult to live on anywhere but nearly impossible as a living wage in NYC. Starting pay for cops is $42,500 and $45,000 for firefighters. Pay for EMS is tops out at $50,000 while fire and police can earn $100,000 or more as they advance.[6] Why aren’t EMS first responders compensated for what they do on the same scale as these other lauded first responders?
Lastly, the depth and difficulty of EMS roles is largely misunderstood, which can lead to underappreciation and underpayment. Despite efforts to raise the profile of EMS practitioners, EMTs and paramedics are still rarely viewed as integral contributors and providers within the overall healthcare system. EMS workers are often the first line of defense in keeping populations alive, especially in the face of crises like the opioid epidemic. Or take for example the Eagle Pass Fire Department in Texas, which is spending tens of thousands of dollars per day taking care of migrants who’ve crossed the southern border – without any federal assistance.[7]
The underpayment of EMS providers is a complex issue that is influenced by an equally complex ecosystem of factors, including the funding structure of EMS agencies, resistance to formal education, discrimination, widespread ignorance of the high-risk nature of the work, minimal certification requirements, and a lack of understanding and appreciation for the role of EMS workers as a vital component of public safety. It’s going to take a massive effort on the part of EMS agencies, their allies, and their constituents to change these misconceptions.
Sources
To Balance Bill or Not to Balance Bill: One Agency’s Decision to Change
Amid the fervent chatter around the No Surprises Act and the final meeting of the federal advisory committee on Ground Ambulance and Patient Billing (GAPB), Digitech has completed an analysis on the impact on a municipal agency that voluntarily ceased balance billing practices in cases where insurance companies did not allow the full charges. Digitech found that the financial impact was modest, but would we advise ambulance providers to stop balance billing patients when commercial insurance plans disallow some of the charges? Read on.
The white paper will:
- Analyze collections data from before and after this policy was in place
- Provide some insight into how ceasing balance billing might impact a broader set of agencies in the EMS industry
- …and more.
To download a complimentary PDF copy of this 10-page white paper, click here.
Webinar: Best Practices for EMS Providers Now That Mandatory Cost Reporting is Underway
Some EMS providers remain unaware that ALL ground ambulance providers are required to provide cost data to CMS, and the first reporting period is already underway. Even if you understand the submission requirements, there are still some best practices to learn that can help the process run more smoothly. In this webinar, Digitech’s cost reporting experts as well as client guest speakers will review the current state of the mandatory cost reporting cycle, share examples and tips from EMS providers’ experiences in the field, and offer insights and resources that will help you avoid the 10% Medicare penalty that CMS will impose if data is not collected and reported accurately.
View the webinar below:
Download the slides here.
Check out our recent blog post if you would like to learn more: CMS Cost Reporting in 2023 and the Impact on EMS & Ambulance Medicare Reimbursement: Where Are We Now?
Innovative Technology in the Face of Crisis
As the first line of defense in our communities, EMS personnel need support now more than ever. Agencies and organizations across the country are pooling their resources to help serve and make a positive impact during this crisis.
Sullivan County Emergency Medical Services, the primary EMS provider for Sullivan County, TN, provides aid to about 150,000 citizens and visitors, as well as those in surrounding communities. A number of ambulances and first responder agencies spread across Sullivan County are ready to respond at a moment’s notice, as their mission is to provide “the best emergency and non-emergency care to patients and their families at the worst times in their lives.”

The progressive care provided by the service personnel of Sullivan County EMS (SCEMS) is often described as an “extension of the emergency room,” where the years of experience offered by the County’s personnel of highly-trained Medical Directors, Paramedics, and EMTs allow them to maintain a “continuity of care from the place of origin to the hospital.” Since 1970, it has been their prerogative to have as many trained personnel on scene of an emergency as soon as possible.
In this particular line of work, “seconds count,” and Sullivan County EMS has committed to having the right systems in place in order to lower response times to medical emergencies within their growing communities. Part of their ability to provide such timely service is due to Sullivan County’s tiered response system, which allows for readily-available, localized teams to respond preemptively:
“These response teams bring manpower and multiple levels of training –from Medical Doctors to First Responders– to the crisis environments faced by our Paramedics and EMTs quickly and efficiently. These teams are highly lauded amongst emergency medical personnel for their selfless acts. With their short response times, they have repeatedly induced appropriate care and –most importantly– prolonged viability of life in the field prior to our arrival.” – Gary Mayes, Regional Director
Sullivan County EMS is not alone in providing care and support for their people. In this rural community, EMS is a third service for the County, acting as an extension of the Sullivan County Regional Health Department (SCRHD). The SCRHD also helps to prepare the County for public health emergencies. Their Public Health Emergency Preparedness Department, recognized by NACCHO Project Public Health Ready, uses “an all-hazards approach for emergency planning, focusing on situations that specifically affect the health of the public.” The SCRHD serves the communities of Kingsport, Bristol, Bluff City, and Piney Flats within Sullivan County. Their department’s workforce of around 90 personnel also works closely with the Northeast Tennessee Healthcare Preparedness Coalition in preparing their response to public health emergencies like the one we are experiencing today.
The collaboration between Sullivan County EMS and their Health Department combined with their support from Digitech as an EMS billing partner has inspired inventive measures to combat the COVID crisis. As technological innovation is at Digitech’s core, the evolution and design of new tools in the Ambulance Commander software system ensures that partners will have access to such timely solutions. With data gleaned from Digitech’s recent COVID-19 Symptom Map, Sullivan County has been able to identify the areas within their community in the greatest demand of care. This insight allows them to strategically place future COVID-19 testing sites, so Sullivan can continue to support their most vulnerable populations.
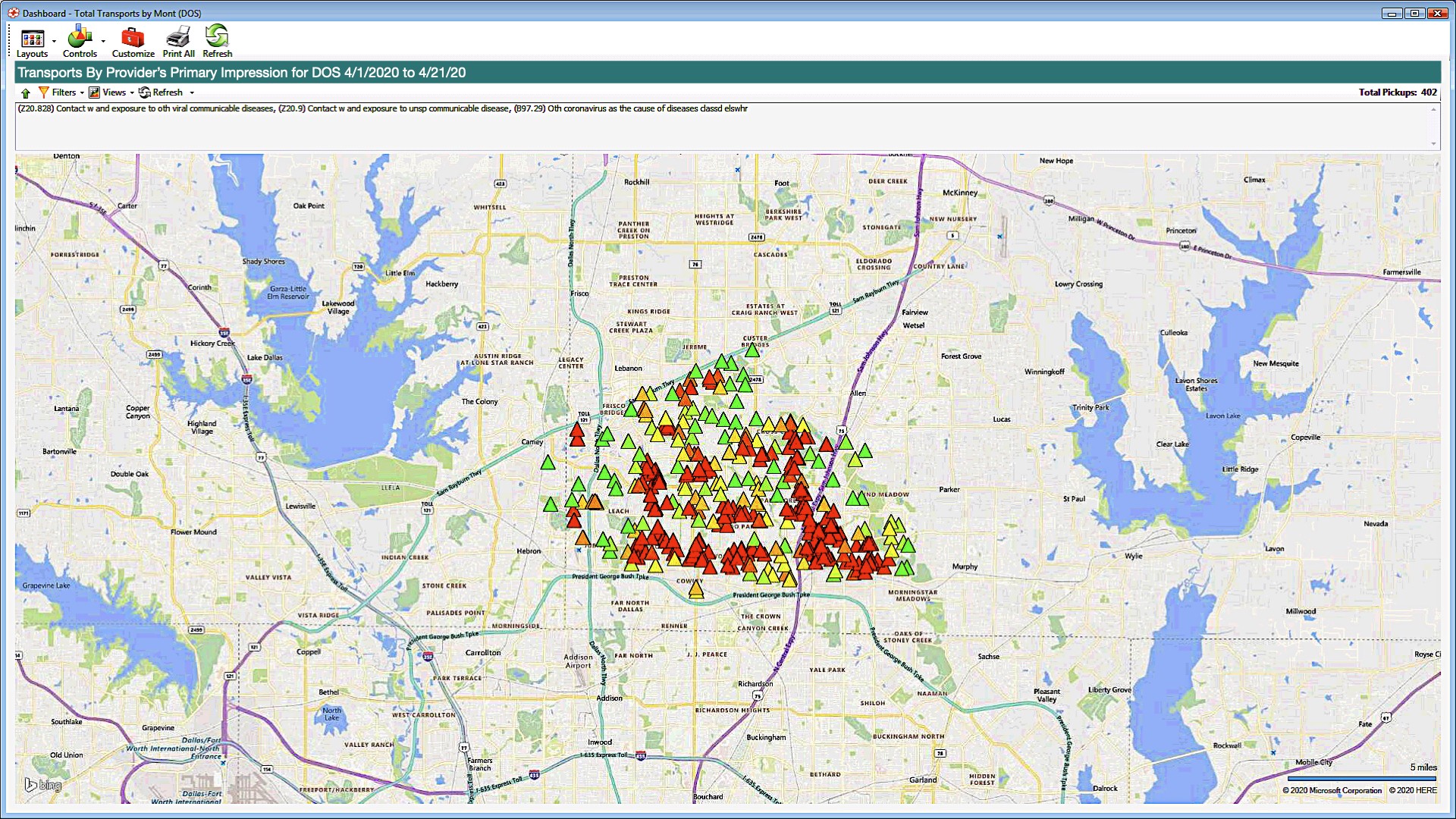
“The COVID Symptom map can be a helpful tool in mitigating the virus by determining specific communities that may need testing, quarantine, or treatment. It allows EMS and Health departments to work collaboratively during the COVID Pandemic.” – Brandon Alley, Sullivan County EMS
The gears continue to turn in Sullivan County as leaders look to this new Ambulance Commander tool for even more creative solutions in the future, like tracking flu-related incidents.
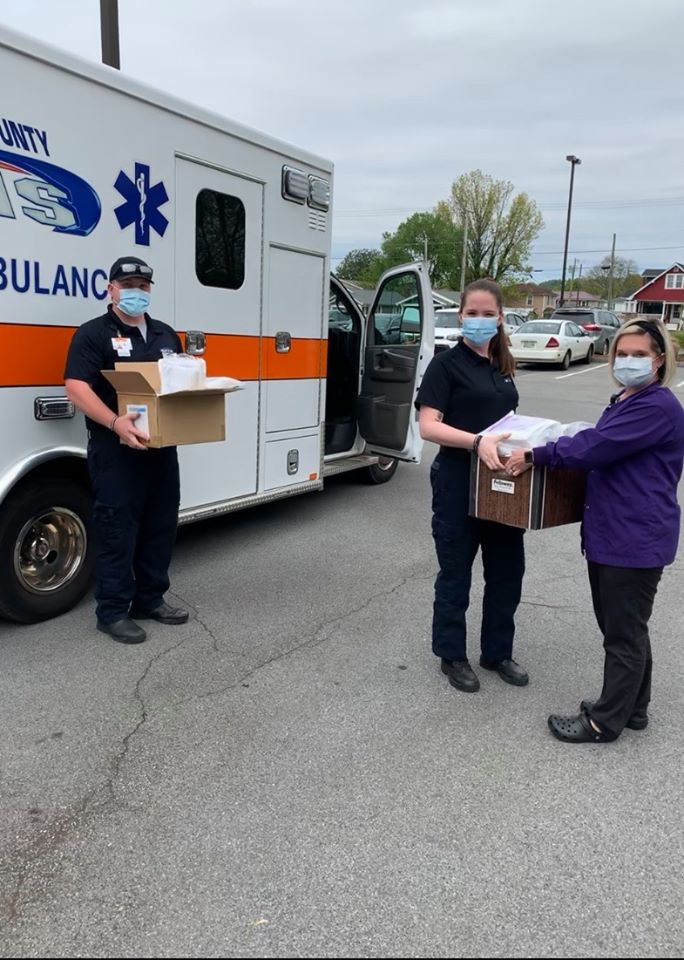
Between these partnerships and updating their Facebook page with information and guidelines on COVID-19, mental health tips, and to thank individuals making donations to support their emergency service providers, Sullivan County EMS continues to commit to their mission of looking out for every single one of their neighbors in need.
Sources:
- Sullivan County EMS, http://www.sullivancountyems.org/main/
- Sullivan County EMS, “First Responders.” January 7, 2015. http://www.sullivancountyems.org/main/section/first-responders
- Sullivan County EMS, “Emergency Services.” January 7, 2015. http://www.sullivancountyems.org/main/section/emergency-services
- Sullivan County Regional Health Department, “History.” 2017. https://www.sullivanhealth.org/about-us/history
- Sullivan County Regional Health Department, “Emergency Preparedness.” 2017. https://www.sullivanhealth.org/emergency-preparedness
- The Northeast Tennessee Healthcare Preparedness Coalition. 2020. http://nethealthcoalition.org/
- Digitech Computer. 2020. https://digitechcomputer.com/.
- Digitech Computer, “New Utilities in Ambulance Commander.” April 24, 2020. https://digitechcomputer.com/new-utilities-in-ambulance-commander/
- Sullivan County Emergency Medical Services Facebook Page https://www.facebook.com/SCEMSOfficial/
New Utilities in Ambulance Commander
Coronavirus Incident Tracking Tools
Our ability to adapt to an ever-changing EMS landscape is a benefit to our clients. We’ve released new tools to help track Coronavirus-related incidents in your service area.
With this latest development, Incident Mapping allows you to:
• Isolate incidents by diagnosis code
• Get a color-coded visual map of your service area’s hotspots
• Interactive maps allow you to drill down to the individual call record
• Adjustable settings to scale heat map coloring based on call volume and service area geography
• Built in integration with Triage utility to display COVID-related pickup locations regardless of provider’s impression
Reach out to your account manager for detailed training by clicking here.
Important COVID News
From all of us at Digitech,
For the duration of this Public Health Emergency, we remain committed to assisting the EMS community by sharing important, up-to-date information with all of our friends and partners. Keeping our clients informed on the most recent updates related to COVID-19 continues to be a top priority. Below is a list of important COVID-19 related industry changes:
- CARES Act Provider Relief Fund – legislation has passed that provides $100 billion in relief funds to healthcare providers on the front lines of the coronavirus response. Due to the importance of delivering the funds expeditiously, the Department of Health and Human Services (HHS) is distributing $30 billion of the relief funds immediately. Please find a summary of the program below. Click here for more details.
- The payments are not loans and will not need to be repaid.
- Payments will automatically be received if your organization received Medicare (FFS) reimbursement in 2019.
- The payments will be received via ACH with a payment description of “HHSPAYMENT”
- Within 30 days of receipt of payment, providers must either accept the payment by signing an attestation and accepting the Terms & Conditions or contact HHS and remit the payment as instructed
- HHS has provided a formula for an estimate of the amount expected which is the amount paid by Medicare in 2019 divided by $484 billion and multiplied by $30 billion. Please contact Digitech if you would like assistance with calculating your estimate.
- The CARES Provider Relief Fund Payment Attestation Portal is now available through hhs.gov/providerrelief.
- Medicare FFS Sequestration Suspension – The CARES Act has temporarily suspended the 2% payment adjustment currently applied to all Medicare FFS claims due to sequestration. The suspension is effective for claims with dates of service from May 1 through December 31, 2020. Providers can expect to receive an increase of 2% more in their Medicare payments during this time period as compared to prior to the suspension.
- Beneficiary Signature Rule Change – Crew members can now obtain a “verbal consent” from the patient to sign on behalf of a suspected or known COVID patient. It is important to note that an actual patient signature is still required in the event the patient is physically or mentally capable of signing and is not a suspected or known COVID patient. Click here for more details, and here for an updated signature form.
- Alternate Destination – CMS has temporarily expanded the list of allowable destinations for ambulance transports to include any destination that is able to provide treatment to the patient in a manner consistent with state and local EMS protocols.
- Accelerated Payment Process – In order to increase cash flow to providers of services impacted by COVID-19, CMS has expanded the current Accelerated and Advance Payment Program to a broader group of Medicare Part A providers and Part B suppliers. The expansion of this program is only for the duration of the public health emergency. It is important to note that these payments are subject to recoupment. Click here for more details.
- CMS Relaxes Physician Certification Statement Signature Requirements – The Centers for Medicare & Medicaid Services (CMS) has released guidance that recognizes the difficulty ambulance service providers and suppliers may have during the COVID-19 Public Health Emergency (PHE) in obtaining a physician certification statement (PCS) signed by a physician or other authorized professional. CMS and its contractors by extension will not deny claims during a future medical audit even if there is no signature for non-emergency ambulance transports, absent an indication of fraud or abuse. Ambulance service providers and suppliers should indicate in the documentation that a signature was not able to be obtained because of COVID-19. The AAA advises completing the PCS form and then indicating if a physician or other appropriate person has not signed it by writing “COVID-19 Public Health Emergency” on the signature line. CMS also reminds providers and suppliers that medical necessity still needs to be met. The full Q&A document can be accessed here.
If you have any questions at this time, please reach out to us.
Solving the Deductible Dilemma with Automation
At Digitech, we don’t see problems—we see opportunities. When a client brings us a question or a problem, we turn it into a challenge. How can we develop a solution that will become a benefit to all who we serve? Can we increase efficiency? Can we write new software that eliminates a roadblock? Can we chart a path through the maze that will lead others out of the same trap?
Take the problem of increasing deductibles in healthcare insurance programs. With costs for health insurance pushing a greater portion of the burden onto the patient, it’s naturally gotten harder to collect ambulance billing claims. Some billing companies might shrug and say, “Well, we’re just going to have to live with a reduction in insurance collections and an increase in self pay claims.”
Not here.
At Digitech, we got to work. We’ve rolled out new automation that enables our verification process to check the deductible information on commercial insurance coverage on a case-by-case basis. For those payers that provide this information, it will be captured in the claim record and will allow us to see whether that claim will hit the patient’s deductible. When a significant portion of the bill may get pushed to the patient, we can hold the claim for a period of time to allow for a greater chance for the deductible to be met. This process is in addition to our standard process of holding Medicare and some Medicare HMO claims for deductibles.
The goal here is the one that Digitech always pursues, while keeping a sharp focus on compliance: Maximized revenue for clients and minimum distress for patients.
Going forward, all Digitech clients can opt in to this program. We’re ready for you! Please reach out to your account manager at Digitech to opt in to deductible eligibility checks and we will get the ball rolling for your service.
You may also contact the Digitech team at accountmanagers@digitechcomputer.com.
Collection Improvement Examples
Digitech has increased revenue recovery for our clients every time we have been contracted. Click on “Before” and “Digitech Year 1” to see how much.
