Digitech’s 2025 calendar keeps rolling with a robust lineup of EMS conferences in Q3. These events offer an opportunity to engage with EMS leaders, exchange ideas, and highlight how our billing solutions can help agencies thrive. Take a look at where we’ll be this quarter!
Reach Out to Our Team
Meet Digitech at EMS Industry Events – Q2 2025
Digitech continues its 2025 journey with a packed schedule of industry-leading conferences in Q2. These events are our chance to connect with EMS professionals, share expertise, and showcase how our billing solutions support agencies nationwide. Check out where we’ll be this quarter!
Reach Out to Our Team
Webinar – The Business of Saving Lives: Balancing EMS Costs and Revenues
Did you miss our latest webinar with JEMS and Fire Engineering? Watch the video recording below of The Business of Saving Lives: Balancing EMS Costs and Revenues, a panel discussion on the financial realities of EMS today.
In this session, industry experts examine the growing financial pressures on EMS agencies and the strategies they use to stay operationally strong. Panelists explore key funding models, whether tax-based or direct billing, while sharing insights on cost management, revenue diversification, and service optimization. Through real-world examples and a dynamic Q&A, the discussion provides actionable takeaways to help EMS leaders improve financial sustainability and navigate reimbursement challenges.
You can watch the webinar here:
Get a demo of our EMS billing platform. Schedule a Demo
Meet Digitech at EMS Industry Events – Q1 2025
Digitech is kicking off 2025 with a packed schedule of industry-leading conferences. These events are our chance to connect, share expertise, and explore the latest in EMS and revenue cycle management. Check out where we’ll be in Q1 below.
Get a demo of our EMS billing platform. Schedule a Demo
Webinar – Fueling the Future of EMS: Exploring Sustainable Funding for Mobile Integrated Healthcare
If you missed this free webinar, we hosted in conjunction with National Association of Mobile Integrated Healthcare Providers (NAMIHP), view it here!
Join these EMS industry leaders for a dynamic webinar on innovation and sustainability in mobile integrated healthcare (MIH). Panelists will share real-world funding models and success stories, followed by a Q&A session for direct insights from the experts.
Speakers:
- Maggie Adams, President, EMS Financial Services, Inc.
- Michael Mason, Section Chief, San Francisco Fire Department
- Kevin Spratlin, Division Chief, Memphis Fire Department
- Lauren Young-Work, LCSW, MIH Coordinator, Palm Beach County Fire Rescue
Moderator:
Michael Brook, Senior VP of Client Relations, Digitech
Webinar – The Hype and the Hope: Exploring Artificial Intelligence in EMS
Did you miss the webinar that we hosted through Pinnacle? Check out the video recording below of The Hype and the Hope: Exploring Artificial Intelligence in EMS, a panel discussion exploring the impact of artificial intelligence in emergency medical services.
In this session, we delve into early uses of AI in EMS, beginning with an overview what AI is – and what it isn’t. Panelists explore AI’s application in their areas of specialization: dispatch and communications, ePCR and RMS software, EMS education, and revenue cycle management. A lively Q&A with the expert panelists offers additional insights and takeaways on the emerging applications of AI in EMS.
You can watch the webinar here:
Or download the slides here.
Beware of Breaches: Data Security Strategies for EMS Agencies
In the fast-paced world of EMS, efficient communication and seamless access to critical information are second only to patient care. As technology continues to revolutionize EMS, securing against data breaches becomes an essential concern. Cyberattacks can lead to damaging consequences, such as a recent ransomware attack that affected computer systems and caused the closure of emergency rooms and redirection of ambulance services in multiple locations[1]. When it comes to protecting sensitive patient data, EMS personnel have not only a legal obligation but also a responsibility to maintain trust and provide high-quality care. EMS breaches can lead to identify theft, which can be damaging to individuals who may already be experiencing the financial and emotional stress of medical emergencies.
Here we explore strategies for EMS leaders to improve data security in their organizations and ensure patient confidentiality while embracing technological advancements.
Vendors’ Security Policies and Practices
Most EMS agencies utilize third-party software or services of some kind these days – ePCR and CAD applications, billing services, hardware manufacturers, and more – and it’s crucial to assess the security measures of those vendors. Ensure that they follow stringent data security practices and comply with industry standards and regulations and have a comprehensive understanding of how vendor relationships impact the security of patient data. All the following strategies apply not just to your EMS agency but to your vendors as well.
A recent data breach that affected numerous EMS agencies was traced back to a third-party vendor’s use of MOVEit Transfer software[2]. Digitech implements stringent security policies and rigorously safeguards our clients’ data. Click here to talk to a Digitech expert to learn more.
Implement Robust Encryption
One of the foundational steps in securing EMS data is the implementation of strong encryption protocols. Encryption scrambles sensitive data, making it virtually impossible for unauthorized individuals to access or interpret. Ensure that both data at rest (stored data) and data in transit (data being sent or received) are encrypted using modern encryption algorithms. This prevents unauthorized access in case of a data breach or theft.
Access Control and Authentication
Access control is the first Technical Safeguard Standard of the HIPAA Security Rules. Implement stringent access controls to restrict data access based on roles and responsibilities. Not everyone in EMS requires access to all patient records. Utilize role-based access control to ensure that each team member can only view or edit the information they need for their specific tasks. Multi-factor authentication adds an extra layer of security by requiring users to provide multiple forms of verification before accessing any systems that house patient data.
Regular Training and Education
Human error remains a significant factor in data breaches. Conduct regular training sessions to educate EMS staff about the importance of data security, best practices for handling protected health information, and the potential risks associated with mishandling data. Make sure all employees are well-versed in recognizing phishing attempts and understand their role in maintaining data security.
Secure Mobile Devices
In EMS, mobile devices play a crucial role in accessing patient information in the field. However, these devices can also be vulnerable points of entry for cyber attackers. Ensure that all mobile devices used by EMS personnel are equipped with strong security measures, such as device encryption, remote wipe capabilities, and biometric authentication.
Regular Software Updates and Patch Management
Outdated software is a common entry point for breaches. Regularly update the operating systems, applications, and software used within EMS to ensure that security vulnerabilities are patched. Implement a systematic process for monitoring and applying updates promptly.
Data Backup and Recovery
Having a robust data backup and recovery plan is essential in case of a cyber incident or breach. Regularly back up all patient data to secure off-site locations and understand the guidance on HIPAA and cloud computing. Test the restoration process periodically to ensure that backups are functioning properly and that critical data can be quickly recovered.
Data Minimization and Retention Policies
Collect only the necessary patient data and avoid gathering excessive information. Implement data retention policies that define how long patient data should be stored and when it should be securely deleted. This reduces the amount of data that could potentially be exposed in the event of a breach.
Audit Trails and Monitoring
Implement comprehensive audit trails that log all activities related to patient data access and modification. Regularly monitor these logs to detect any unusual or unauthorized activities. Anomalies can be identified and addressed promptly, minimizing the potential impact of a security breach.
Incident Response Plan
Despite the best preventive measures, security incidents can still occur. Having a well-defined incident response plan in place is essential. This plan should follow the HIPAA Breach Notification Rule and outline the steps to be taken in the event of a data breach, including notifying affected parties, addressing the breach’s root cause, and implementing measures to prevent future incidents.
Conclusion
Technology advances bring with them the responsibility of safeguarding sensitive patient data. By implementing a robust combination of encryption, access controls, staff training, and comprehensive security practices, EMS providers can ensure the confidentiality and integrity of patient information. As the healthcare landscape continues to evolve, so too must our commitment to data security in the realm of EMS.
[1] https://www.cbsnews.com/news/prospect-medical-cyberattack-california-pennsylvania-hospital/
Webinar: Best Practices for EMS Providers Now That Mandatory Cost Reporting is Underway
Some EMS providers remain unaware that ALL ground ambulance providers are required to provide cost data to CMS, and the first reporting period is already underway. Even if you understand the submission requirements, there are still some best practices to learn that can help the process run more smoothly. In this webinar, Digitech’s cost reporting experts as well as client guest speakers will review the current state of the mandatory cost reporting cycle, share examples and tips from EMS providers’ experiences in the field, and offer insights and resources that will help you avoid the 10% Medicare penalty that CMS will impose if data is not collected and reported accurately.
View the webinar below:
Download the slides here.
Check out our recent blog post if you would like to learn more: CMS Cost Reporting in 2023 and the Impact on EMS & Ambulance Medicare Reimbursement: Where Are We Now?
CMS Cost Reporting in 2023 and the Impact on EMS & Ambulance Medicare Reimbursement: Where Are We Now?
Check out our webinar on this topic: Best Practices for EMS Providers Now That Mandatory Cost Reporting is Underway
Mandatory CMS cost reporting was announced in earnest several years ago, only to be interrupted and delayed (like many things in our lives) by the COVID Public Health Emergency. Now, ground ambulance providers are focused on reporting under the Medicare Ground Ambulance Data Collection System (GADCS), with approximately half of all EMS agencies well into or even having newly completed their mandatory data capture. The other half of EMS agencies are at the beginning stages of collecting the required data. The process of data submission to CMS has just begun, depending on the reporting period for each agency.
Now is a good time to take a look at some of the context around mandatory CMS cost reporting and examine the impacts on Medicare reimbursements in the medium-term as a result of these efforts.
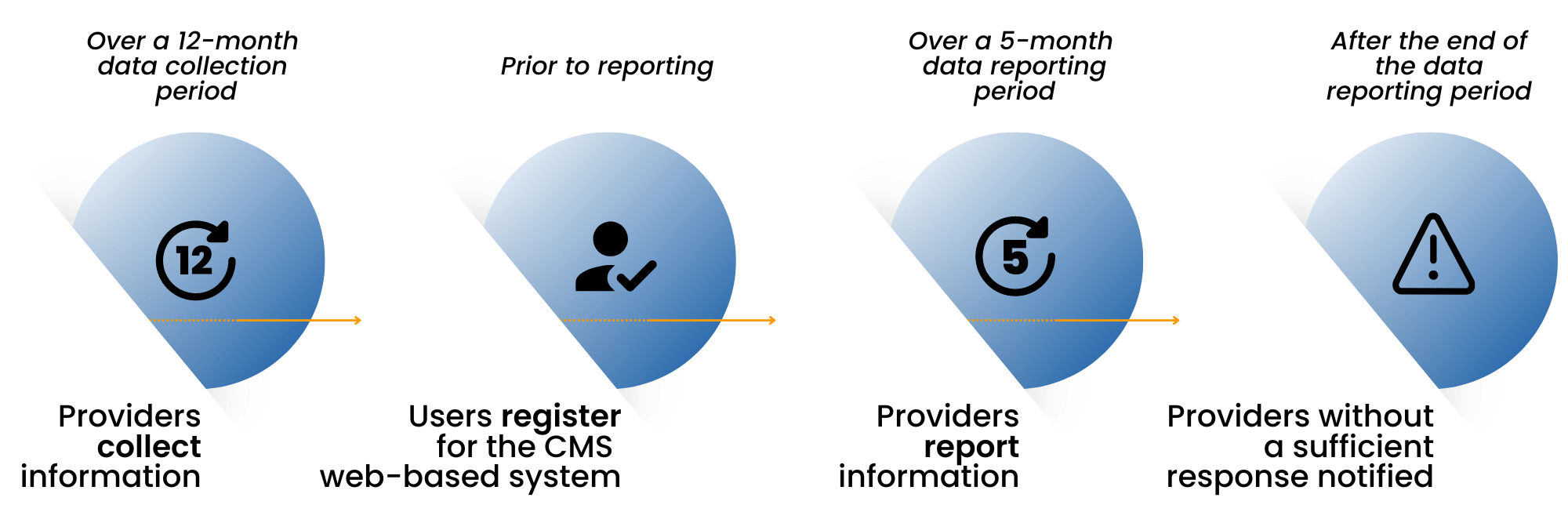
GADCS Key Milestones for EMS Providers
First, let’s review the history of ambulance reimbursements and how the structure for ambulance reimbursements differs from the reimbursement allowables that Medicare sets for other healthcare services.
In 2002, Medicare implemented a phased-in national fee schedule for ambulance services. The goal was to address the high variability in the amounts being reimbursed depending on whether an EMS provider was hospital-based or independent. In 2005, the Government Accountability Office (GAO) conducted a cost study. Interestingly, of the responses received in the cost study, 1/3 were omitted because the responding services were Fire-based and did not have a clean carveout of only ambulance costs versus other costs. The GAO report estimated that in 2010, excluding most Fire based agencies, 39-56% of providers would receive average Medicare reimbursement payments that would exceed their costs – which means, conversely, that half or more of the providers would not be able to cover their costs with Medicare’s reimbursements (Ambulance Providers: Costs and Expected Medicare Margins Vary Greatly, 2007). Additionally, the GAO report identified super rural providers as being at the highest risk of having Medicare payments well below their costs.
In an attempt to address the perceived shortfall in Medicare reimbursement, Congress included temporary Medicare ambulance bonus payments in the Medicare Modernization Act that paid an additional 2% (urban), 3% (rural), and 22.6% (super rural), starting in 2004. Those temporary bonus payments have been extended, with much debate, every few years since then.
Elsewhere in healthcare services – hospitals, physicians, clinics, labs – Medicare payments are established via an annual collection of cost data from all providers. CMS uses the collected data to update the allowable amount continually to cover costs for the provider, plus a reasonable margin. Ambulance services have been the exception, and the industry has been vocal about the existing allowables not being sufficient to cover the costs of providing the service. Outside of the 2005 GAO study, which excluded a large number of fire-based municipal ambulance providers, there is little factual data that ties current reimbursements to current ambulance rates. The amounts set in 2002 are adjusted by an annual inflation factor. The “temporary” Medicare add-on bonus payments are a modest recognition that the current Medicare rates are insufficient.
As you likely have inferred, the ambulance cost reporting initiative by CMS is intended to put ambulance providers on par with other healthcare service providers in terms of assessing costs and delivering fair reimbursement. EMS providers have received a concession, at least initially, by not being required to submit cost data annually, but rather every four years.
The collected and reported data is going to the Medicare Payment Advisory Commission (MedPAC); MedPAC will then be required to submit a report to Congress on the adequacy of Medicare payment rates for ground ambulance services and geographic variations in the cost of furnishing such services. The timing of that report is not specified. The idea is that, at some point in the future, the data would be used for resetting the amounts Medicare will pay to ground ambulance providers.
There has been speculation by some providers that the Medicare allowable amounts will go up significantly as a result of the cost reporting submissions, while others believe the amounts could drop. This difference in perspective likely depends on what type of agency you are. Fully integrated providers under municipal structures typically have costs substantially higher than the current allowables, but private ambulance services that provide a large percentage of 911 services nationwide typically have a much lower cost structure. Also, agencies running all-ALS services have a higher cost structure than those that have a mix of ALS and BLS vehicles in their system.
No matter what, over the next several years, we expect to see changes to Medicare reimbursements in ground ambulance as a result of the cost reporting efforts. Generally the sentiment is that, at minimum, the cost of providing 24/7 911 services has increased faster than the current inflation factor accounts for. Time will tell, but there is a reasonable chance that reimbursements will be enhanced to better align with today’s costs of providing this critical service.
Digitech hopes that you find this context about the substantial Medicare GADCS cost reporting effort useful to understand the system more deeply or to explain the reasons to your key stakeholders. Please reach out to CMSDataCollection@digitechcomputer.com if you would like more information about Digitech’s data collection software, which assists agencies in organizing the required data elements, or if you would like assistance in data collection via our cost reporting consulting services.
—
Check out our webinar on this topic: Best Practices for EMS Providers Now That Mandatory Cost Reporting is Underway
Three Tactical Strategies to Improve Reimbursement While Maintaining Quality Clinical Care
Have you ever been asked to “do more with less”?
It’s not easy to be an EMS provider these days. Whether it’s increased expenses, decreased funding, or payers taking a harder stance on reimbursement, EMS agencies across the nation are faced with challenges when it comes to maximizing revenues. In this whitepaper, we focus on three strategies that aim to improve your organization’s revenue cycle without cutting staff or changing your patient care processes. Download the complimentary whitepaper here.
Why Should You Outsource EMS Billing?
EMS billing isn’t for the faint of heart. While patient care is the core mission of any EMS organization, it’s impossible to provide adequate care without resources provided by a healthy revenue stream.
Billing Isn’t Just Paperwork
Agencies that handle their billing in-house, rather than outsourcing EMS billing to a third-party vendor, are in fact running two business. Ambulance transport and EMS billing are different enterprises with different requirements for staffing, IT infrastructure, compliance, operational costs, analytics, and more.
This leads many EMS agencies to outsource their billing. Smart decision. The fee that a billing service will charge will certainly be less than the cost of running a second internal business. Let a specialized company handle the specialized work of billing so that the EMS agency can focus on patient care and other operational priorities.
Here are five main reasons why EMS agencies have made the switch to outsourcing.
1. Reduced Costs
An established third-party billing company has a head start on infrastructure that an in-house department may never catch up with. Staffing, workspace, IT, hardware, training, software licenses, maintenance, even office supplies and equipment – these essential elements create burdensome ongoing fixed costs. Letting the billing provider handle these costs allows the EMS organization to direct resources to other essential budget items. Meanwhile, if the billing company invests in scaling their operation, building technology, and attracting top-tier staff, those benefits will be passed along to clients.
2. Industry Expertise
Billing companies deal with hundreds of providers, payers, and facilities – far more than a single EMS organization with an in-house billing department ever will. You may transport to a few different hospitals, but a billing firm may have connections to hospitals across an entire region and access to databases of patient data that your in-house billing team will not have. Outsourcing EMS billing allows you to take advantage of these economies of scale and collect every dollar.
Billing vendors also have the benefit of a broader range of resources and staff who can engage with industry associations, attend events, and stay abreast of trends in the changing healthcare environment. A good partner will keep you informed of new developments when necessary and will make sure that changes are incorporated into technology and policy as needed.
3. Top-Tier Technology
All billing companies rely on claims processing software to manage their operations. Good billing companies develop their own claims processing software to manage their operations with efficiency, opportunities for customization, and automated processes balanced with manual oversight.
Simply put, it would be impossible for an in-house billing department to develop and scale the technological expertise needed to maximize the potential of technology for billing.
4. Customer Service for Patients
After a traumatic 911 event, the best customer service may be no customer service at all. In other words, the best thing for a patient is not to have to worry about how to pay for their emergency transport.
Often, individuals are confused about their insurance coverage for EMS services. Third-party billing companies have advanced technology solutions designed to identify patient insurance information quickly and efficiently – more so than an in-house billing department could do alone, even armed with the best software. If your billing company processes millions of claims annually, they have established manual and automated processes to uncover patients’ insurance information through clearinghouses, demographic databases, admitting hospital data access, and sheer manpower.
Patient inquiries and other sensitive customer service touchpoints will inevitably still arise, so it’s important to look for a third-party vendor with high levels of professionalism and sensitivity to your organization’s reputation.
5. Increased Collections
The results of the combination of cost reduction, industry expertise, targeted technology, and great customer service? Increased collections for your organization. A billing company has one goal: maximizing the return on every claim submitted. To keep the business viable long-term, they must do so compliantly and direct resources toward infrastructure and technological innovation. This results in increased collections for clients.
Third-party billing companies should also have the capability to perform sophisticated analysis by looking at the right metrics to measure performance. Your billing partner should help you understand the right data at the right time for the right reasons. Then, you’ll be able to monitor and assess your billing company as well as project revenues.
Deciding how to handle your agency’s EMS billing takes analysis and careful consideration, with plenty of pros and cons to weigh. We’ve provided a handful of good reasons to outsource EMS billing. What are your reasons to keep doing your own billing?
Webinar: The State of Mobile Healthcare 2022
This free panel discussion with Pinnacle explores the current state of affairs in Mobile Integrated Health: the ET3 rollout, the regional and local disparities in the execution of mobile integrated healthcare, and how providers are overcoming the many challenges to efficient delivery of mobile health services. The expert panelists also share perspectives on where we’re headed and provide some guidance.
View below:
Speakers:
Michael Brook, MBA
Jonathan Washko, MBA, FACEP, NRP, AEMD
Dr. Allen Yee
Dr. Victoria Reinhartz, CPh
Dr. Marc Eckstein, MD, MPH, FACEP, FAEMS
Check out this page for some Mobile Integrated Health Resources.
Webinar: Ethical Partnerships With Third-Party EMS Vendors
The business world is built upon relationships. Relationships are the building blocks of the partnerships and contracts that keep all businesses running.
EMS is no different. You can’t do it alone. From medical equipment to apparatus to outsourced billing, partnerships with third-party businesses are essential to EMS agencies. But if those relationships aren’t built upon an ethical foundation, neither party will truly thrive.
We recently covered this important issue in a webinar hosted by Pinnacle’s Webinar Series. Our Executive Director of Analytics and former Battalion Chief at Gwinnett County Fire and Emergency Services in Georgia, Mitchel Holder, was joined by Nathan Sweet, Director of EMS at Anderson County, Tennessee, to discuss forging ethical partnerships with third-party vendors. Watch the webinar for key strategies and food for thought on this important topic in EMS.
Here’s what you can expect to see:
- What does an ethical relationship with a vendor look like?
- How do you prepare to solicit a new vendor partner?
- How do you establish ethical relationships with vendors?
- What are the standards for ethical business relationships?
- How do you assess a potential partner’s commitment to ethical behavior?
- How does an ethical partner behave when something goes wrong?
- What are the qualities of ethical partner relationships?
50 Questions to Ask on Your EMS Billing RFP
Issuing an EMS billing RFP this year? Selecting the right partner for EMS billing is a crucial decision for every EMS organization that outsources billing services.
Determining the best fit can be daunting. Choose wrong, and it could have devastating consequences to revenue and reputation. Choose right, and you could develop a mutually beneficial relationship with a vendor that helps your agency flourish for decades to come.
Many agencies go through a request for proposal process to find a billing partner, either for convenience and assistance with the search or because they are required by their governing body. Our team here at Digitech is highly experienced in creating proposal responses to these RFPs; we’ve read more than we care to admit over the years. In doing so, we’ve identified a standard set of questions that we believe should be in your next EMS billing RFP, whether you’re considering outsourcing for the first time, you know your department needs a change, or you are seeking to determine if your current provider is still the best fit.
This list arms you with 50 questions in six major areas to include in your EMS billing RFP. Answers to these questions will give you a deep understanding of the proposing vendors so you can make an informed choice.
Want a printable checklist? —> click here
Company Overview
- How many years has your company been in business?
- How many years has your company provided third-party EMS billing services?
- Disclose any key business partners, subsidiaries, and/or contractor relationships.
- How many EMS billing clients do you have and what type are they (e.g. municipal, hospital-based, private)?
- How many EMS claims does your company bill annually?
- How many employees to you have dedicated to EMS billing services?
- Provide an organizational chart providing the roles and responsibilities of the employees who will manage and/or be assigned to perform services.
- How many offices do you have dedicated to providing EMS billing services? Where are these offices located?
- Provide information about your customer service policies and procedures, including escalation and issue resolution processes.
- Describe how your company is notified of changes in legislation and how that information will be incorporated into your systems and processes in a timely fashion.
- List any professional EMS associations that your company belongs to.
- Provide a list of all award protests that your company has filed in the last five years, including the reason for the protest and the outcome.
- Provide contact information, start date, annual transports, and a brief narrative covering implementation and services provided for three current EMS clients of similar size, complexity, and scope.
Compliance and Regulatory
- Does your company have a compliance plan that is updated regularly?
- Is a copy of your compliance plan available for inspection upon request?
- Has your company, its parent, or a subsidiary ever been investigated for suspected fraud and abuse by any department or agency within the federal or state government such as OIG, Medicare, Medicaid, CMS, or Recovery Audit Contractor?
- Has your company, its parent, or a subsidiary ever been required by a department or agency of the federal or any state government to follow a Corporate Integrity Agreement?
- Has there been an investigation where the final determination resulted in a client paying a fine or penalty due to coding and billing actions that were related in any way to your provision of services?
- Are you able to furnish evidence upon request that all current employees are not excluded from participation in state and federal healthcare programs?
- Please provide a brief description of your company’s quality or audit process.
- Is any auditing process provided by an external vendor or source? If yes, briefly describe these audits.
Technology and Security
- Is the EMS claims processing and billing system you use proprietary to your company or is it software developed by a third party?
- Provide a general overview of the billing and records management solution. Describe the billing software used, who owns it, who supports it, how many clients use it, and describe the process by which required programming changes are made.
- List any additional licenses that are necessary to fully operate all available aspects of the proposed billing software, including reporting software.
- What level of access will be provided into the billing system? Will it include full visibility into all actions, notes, documents, etc.?
- Does your system provide logging of all activities on a patient account for all dates of service, and do you provide access to these logs?
- How is patient information stored, and for how long is this data retained? Are these records retrievable by the client?
- Please provide a brief description of your business continuity plan or disaster recovery plan.
- Provide a detailed listing of all data breaches including volume of patients affected and current status.
- Provide evidence of at least three years of annual SOC 1 Type 2 audits.
Coding and Billing Process
- What is your preferred method for receiving ePCR information?
- Explain the format that the ePCR data will be uploaded into the billing software, and what fields will be included, e.g. patient demographics, insurance, guarantor, medical procedures performed, chief complaint, dispatched as, and found to be.
- Briefly describe the training process for a new coder that starts with your company.
- How are coding personnel audited?
- How are claims assigned to coders? Are specific coders or groups of coders assigned to certain clients?
- If there is not enough information to code the claim, what is the process for obtaining the necessary information?
- Please describe the circumstances in which a claim would be returned to a client.
- What is the typical length of time required to bill a claim once the necessary information is received?
- What is your standard invoicing process and timeline?
- Describe the appeals and review processes for denied claims and the process for limiting denied claims.
- Describe the cash posting process.
- Describe the refund process.
- Please describe your process, including the frequency, for providing documentation feedback to providers.
Implementation and Onboarding
- Describe the initial phases of this project, including a proposed implementation plan.
- Describe how you ensure that implementation and the transition to your system does not negatively impact the billing and collections processes for our organization.
- What resources will we need to provide during onboarding and implementation?
- Describe the support and training you provide during the onboarding process, and describe the ongoing support and training for our administrative personnel that you will provide once onboarding is complete.
Reporting
- Please provide sample of weekly or monthly client reports that are part of your standard client reporting process.
- How are requests for non-standard reports handled? Is there a cost for these types of reports? If so, how is pricing determined?
- Please include any additional information regarding your reports and the data analysis tools provided to your clients.
We hope this list helps you get started in your endeavor to create or revise an RFP related to your organization’s EMS billing and coding process.
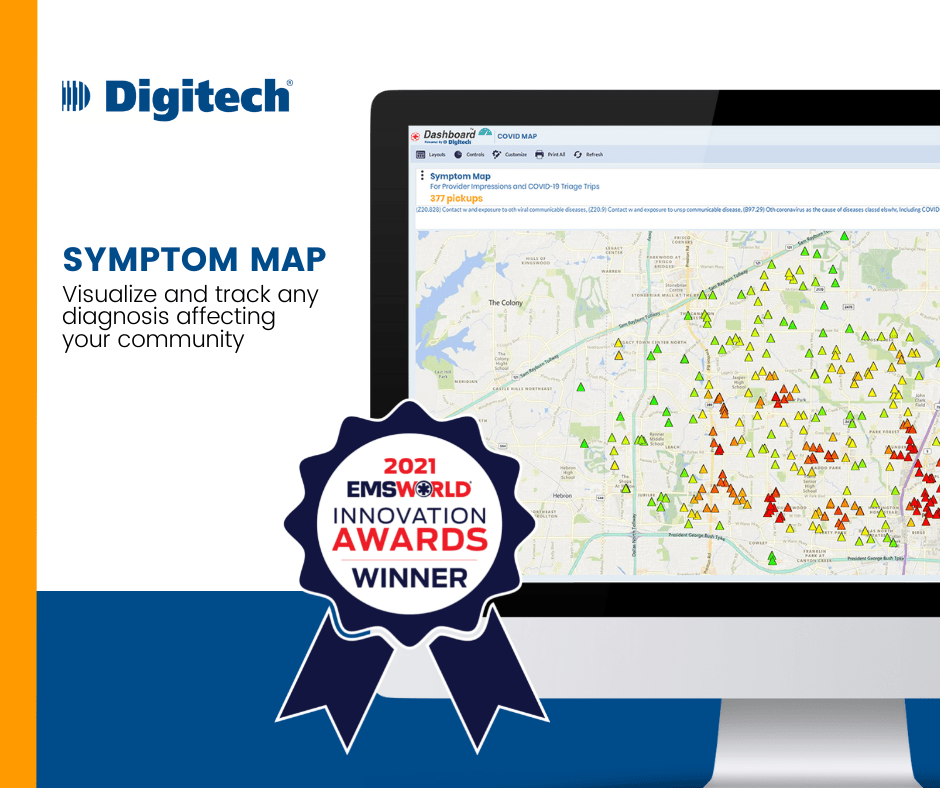
Digitech Wins EMS Product Innovation Award
Interactive symptom heatmap was rapidly developed and deployed to clients at the height of COVID-19
CHAPPAQUA, N.Y., December 6, 2021 – Digitech, the leading provider of EMS billing and technology, is pleased to announce that the company’s Symptom Map solution has been named an EMS World Innovation Awards 2021 winner.
Digitech’s Symptom Map, part of the company’s proprietary billing platform, is an interactive heat map that allows EMS agencies to geospatially track call locations and responding crews. Symptom Map users can track any diagnosis code or provider impression, map the concentration of EMS responses to specific symptoms, and drill into individual claims to see all account details, including the complete patient care report.
The development of Digitech’s Symptom Map was driven by the COVID-19 crisis. In early March 2020, it became clear that COVID-19 would have a significant impact on EMS operations everywhere, and Digitech drew upon its history of rapidly delivering solutions in response to evolving needs. A client approached Digitech with a request to help them understand how and where the virus was spreading within their constituency. The request was swiftly passed to our development team. Within days, Garrett Anger, senior developer at Digitech, had delivered a prototype of the heatmap.
With just a few refinements, the solution was made available to all clients before the end of March 2020, just two weeks after COVID-19 was declared a Public Health Emergency. EMS leaders among Digitech’s client base began to put it to use immediately. For example, Sullivan County Health Department in Tennessee used the Symptom Map to determine where they could most effectively deploy mobile testing stations and maximize resource utilization. Built-in integrations with other tools in Digitech’s technology platform enabled administrators to display COVID-related pickup locations regardless of the provider’s impression.
EMS World holds their esteemed Innovation Awards contest to recognize the most pioneering products of the year that have the potential to transform EMS care. Previously, Digitech won the prestigious award in 2013 for its PCR Lens field data collection aggregation and improvement tool. EMS World Innovation Award judges noted that Digitech’s Symptom Map is “an original and useful way to track health concerns and environmental dangers in a given jurisdiction or patient populations.”
“We are honored to receive the recognition of this 2021 EMS World Innovation Award,” said Walt Pickett, Chief Operating Officer for Digitech. “The award is a testament to Digitech’s continuing commitment to innovation that is responsive to our customers’ needs.”
To view this release as a PDF, please click here. Originally published at newswire.com/news/digitech-wins-ems-product-innovation-award-21570269.
Three Critical Questions About EMS Revenue and Performance
Action is at the heart of EMS: making quick decisions in the heat of the moment that are often truly a matter of life and death.
In the field, the business maxim of “if you can’t measure it, you can’t manage it” doesn’t exactly apply. You don’t expect a medic to pull up an analytical dashboard between calls and begin crunching numbers.
And yet, data analysis plays a huge part – not only in improving patient care and outcomes, but crucially, in the performance of the entire EMS organization. It is critical to understand the available data about challenges, opportunities, and strategy in order to make the best decisions for your agency.
In this whitepaper, we focus on three critical questions for EMS billing. You can use these questions to guide your analysis and assessment of revenue collection performance of your billing department, billing vendor, or billing solution.
- How are you calculating collection percentage – and why?
- How are you analyzing collections per trip?
- How are you measuring efficiency?
Digitech Closes Successful First Quarter Of 2021
Digitech’s Growth Continues Through Customer Acquisitions, New Hires, and Technology Upgrades
Chappaqua, NY, April 27, 2021 – Digitech, a leading provider of EMS billing and technology services, announces that it has closed a successful first quarter of 2021 with key additions to its staff and customer base as well as the continued migration of legacy clients onto their industry-leading billing platform.
“Despite its many challenges, 2020 was a watershed year for Digitech,” said Mark Schiowitz, President and CEO. “We closed a successful Q1 2021 because the stage was set last year. The pivotal event was our acquisition of the R1 EMS business unit in 2020, which required a tremendous amount of preparation and effort from our Digitech teams. Now, we are reaching new milestones as part of our continued commitment to efficiency and innovation.”
Significant Digitech achievements during this quarter include:
- 12 new contracts signed with municipal, private, and nonprofit ambulance organizations, representing $70MM in annual collections to these agencies. This represents a 99% renewal rate with our existing clients and expands our reach with new clients in key states such as Tennessee, Florida, Virginia, and California.
- Upgrading the processing system for clients who are now with Digitech after the R1 EMS acquisition. The upgrade involves migrating client processing from the legacy Intermedix EMR billing software to Digitech’s proprietary platform. By mid-year, Digitech is projecting that 35% of these clients will be converted, resulting in efficiency, revenue gains, and improved access to data.
- Strategic new hires in Digitech’s legal and compliance departments, as well as the growth of new combined teams that bring together the best practices and efficiencies from two companies.
- Coding process advancements and smart automations coming out of our billing and technology teams, leading to an increase in claims processed per hour, while maintaining our track record of impeccable accuracy and compliance.
“We’re excited about the momentum,” said Jason Crowell, Senior Vice President of Sales at Digitech. “Our year-over-year consistent performance and dedication to our clients is resonating in the marketplace. The strides we’ve made thus far in 2021 will help us reach our next stage of growth. More and more EMS agencies are reaping the benefits of Digitech’s strong compliance program, transparent real-time reporting and analytics solutions, and high level of client service.”
To view this release as a PDF, please click here.
Legal Experts Join Digitech to Expand Compliance Team
Chappaqua, NY – March 15, 2021 – Digitech, a leading provider of EMS billing and technology services, has announced that Krina Merchant has been hired as Corporate Counsel and Amanda Stark has been hired as Risk Manager.

Ms. Merchant brings with her a background of balancing business goals with legal risk, which allows her to effectively support departments across Digitech. She recently held a role as corporate counsel for a cutting-edge biotechnology company, and has significant experience working in heavily regulated industries. She holds a Bachelor of Arts from The University of Western Ontario (Canada) and received her Law Degree from The University of Leicester (UK). Subsequently, she earned a Master of Laws from Osgoode Hall School of Law (Canada) and a second Master of Laws from Fordham University. Ms. Merchant is licensed to practice law in the State of New York. She is currently completing training to become a Certified Ambulance Compliance Officer.
Ms. Stark joins Digitech from Page, Wolfberg & Wirth, the nation’s leading EMS industry law firm, where she specialized in Medicare compliance. There, she co-authored the Ambulance Compliance Program Toolkit, created and taught the Certified Ambulance Compliance Officer course, and worked with clients across the country to create and improve their compliance programs. Ms. Stark is licensed to practice law in California. She earned her undergraduate degree from Millikin University, received her JD from the University of Illinois, and is certified in Healthcare Compliance (CHC). As Risk Manager for Digitech, her responsibilities include reviewing and auditing clients’ claims to ensure they are billed in compliance with each payer’s rules.
Mark Schiowitz, President and CEO of Digitech, said, “We’ve always been proud of our impeccable compliance record. As the largest EMS billing firm in the country, we’ve scaled our legal, compliance, and audit teams so that we can continue to serve ambulance agencies of all sizes. We are honored to bring these experienced professionals on board to lead the most rigorous compliance program in the industry.”
To view this press release as a PDF, please click here.
Embracing Change: Writing the Next Page of Digitech’s Story
Today marks a milestone for Digitech. We’ve finalized the merger between the R1 EMS business and Digitech that was announced earlier this year, and we are now moving forward with operations as a combined business under the Digitech name.
As a 36-year-old company, we’ve seen a lot of changes that have impacted our organization in one way or another: the shift from paper dispatch systems to CAD. The creation of NEMSIS. Changing EMS education standards and compliance requirements. Revisions to Medicare’s national ambulance fee schedules. The Affordable Care Act. Advancements in mobile integrated healthcare. The still-evolving response to the COVID-19 pandemic. While some of these occurrences have been more challenging to deal with than others, Digitech thrives on these kinds of changes. Constant adaptation to the continuously changing environment of EMS is at the heart of our success.
Now we embark on a unique milestone for Digitech. Throughout our history, we have added clients and even employees carefully and selectively. Our growth can be attributed largely to strong references and referrals, and we are proud of that strong reputation. Moving forward, we will continue to build upon the mission and vision that R1’s EMS division (formerly ADPI/Intermedix) and Digitech share: compliantly maximizing collections for customers through time-tested processes and powerful technology, keeping revenue flowing so EMS providers can focus on keeping their communities safe and healthy.
This shared dedication brings together two companies that have been competitors for a decade. As we continue under one metaphorical roof, we have a great opportunity to bring the best, most trustworthy ambulance billing services to even more Fire and EMS agencies across the country.
As one business, we bring a deep level of expertise to the marketplace. At Digitech, EMS billing is all we do. We are not part of a larger revenue cycle management company, and we do not have other divisions that focus on different lines of business such as physician billing. This allows us to specialize like no other company can. Our staff is made up of former Fire chiefs, EMS directors, paramedics, EMTs, and other first responders and public safety professionals. We know EMS.
We’ve also always been a technology company. Ambulance Commander will remain the same efficient processing platform that has powered our EMS billing services for years. We’ve always invested heavily in this area, directing our time and resources to improving our proprietary platform’s speed, availability, and transparency. Our in-house teams have spent countless hours on research and development. Digitech’s developers not only continuously incorporate client feedback and fine-tune processes with client goals and needs in mind, but also react instantly to the unexpected, like legislative mandates, reimbursement changes, and public health emergencies. Now, we will be able to dedicate even more of our efforts to Ambulance Commander. We’ll be rolling out more user-friendly features, careful automations, and informative reports.
As we launch into the first merger or acquisition in Digitech’s history, we more than double our staff and customer base. We have a tremendous opportunity ahead of us to expand our reach in the EMS community, to innovate more, to continue our tireless dedication to our mission. Among the many compelling strategic reasons for this transition, we pledge to maintain the same goal we’ve had since 1984: make every client feel like they’re our only client.
The Price of a Pandemic: The Economic Impact of COVID-19 on Emergency Medical Services
The overwhelming impact of the COVID-19 pandemic has not spared EMS. Quite the opposite—EMS and Fire departments continue to deal with grueling challenges since Severe Acute Respiratory Syndrome Coronavirus 2 exploded into the public sphere in early 2020.
While the health impact of COVID-19 has been destructive in many communities across the globe, the economic impact has hit EMS especially hard as well. Per an ongoing survey administered by the International Association of Fire Chiefs (IAFC), Fire and EMS agencies increased spending nearly 30% on COVID-related expenses.
And increased spending is just the beginning.
Click here to continue reading and download the full whitepaper.
Sarnova to Acquire and Simultaneously Combine Digitech and R1 EMS Businesses
Sarnova to Acquire and Simultaneously Combine Digitech and R1 EMS Businesses in Partnership with Pamlico Capital and Digitech Founder & CEO Mark Schiowitz
Combination Creates Leading Emergency Medical Services Revenue Cycle Management Provider
DUBLIN, Ohio, July 20, 2020 — Sarnova announced today that it will acquire and simultaneously combine Digitech and the R1 RCM Inc. (“R1”) EMS business (formerly ADPI/Intermedix), in partnership with Pamlico Capital and Digitech Founder and CEO Mark Schiowitz, to create a leading provider of revenue cycle management (RCM) solutions for emergency medical services (EMS) professionals. The business will continue to operate under the Digitech name and will be led by Mark Schiowitz and the combined management teams.
Sarnova is a leading national specialty distributor of healthcare products and services for the EMS and acute care markets. Sarnova’s Bound Tree Medical division has been a dedicated servant of the EMS community and committed to its mission “to help those who save and improve patients’ lives” for over 40 years. “We are committed to providing an unparalleled portfolio of products and services to our existing and new EMS customers, and this transaction is a significant demonstration of that commitment,” said Jeff Prestel, CEO of Sarnova. “We invest in companies and capabilities that specifically serve the EMS industry with the best products, services, and support,” said Mark Dougherty, Chief Business Development Officer of Sarnova. “We are excited to support Digitech’s growth through continued investment in its innovative technology platform and expansion of its dedicated team of EMS billing experts.”
Digitech, headquartered in Chappaqua, New York and led by Founder and CEO Mark Schiowitz since 1984, offers comprehensive RCM services and technology solutions focused exclusively on the EMS market. Digitech serves municipalities, hospitals, and private ambulance customers through innovative technology, time-tested processes, and true partnerships with EMS clients. “We are solely dedicated to serving the EMS industry with our billing solutions, and we are excited to serve a wider range of EMS providers with the acquisition of the R1 EMS business,” said Mark Schiowitz. “With investment from Sarnova and Pamlico, we have a unique opportunity to bring two great EMS RCM companies together to further support the success of our current and future customers by maximizing their revenue with superior technology, integration expertise, and transparent real-time reporting.”
“We look forward to partnering with Pamlico Capital, Mark Schiowitz, and the Digitech and Sarnova teams to support Digitech’s next phase of growth and advance Sarnova’s commitment to be the partner of choice for the EMS community,” said Yuriy Prilutskiy, Managing Director at Patricia Industries, a part of Investor AB and majority owner of Sarnova.
Pamlico Capital, an investor in Digitech since 2019, will retain a significant interest in the business alongside Sarnova and Mark Schiowitz. “We are incredibly excited to continue our investment in Digitech and we look forward to helping Digitech, in partnership with Sarnova, increase its presence in the EMS industry and continue to innovate its core offerings,” said Art Roselle, Pamlico Partner.
Sarnova was represented by Robert W. Baird & Co. Inc (financial advisor) and Simpson Thacher & Bartlett LLP (legal advisor). Pamlico was advised by Alston and Bird LLP (legal advisor). R1 was advised by Evercore (financial advisor) and Winston & Strawn LLP (legal advisor).
About Sarnova
Sarnova is the leading national specialty distributor of healthcare products in the emergency medical services (EMS) and acute care markets. The company is comprised of four major business units: Bound Tree Medical, Cardio Partners, Emergency Medical Products and Tri-anim Health Services. Sarnova is a company of Patricia Industries, a part of Investor AB, which makes significant investments in best-in-class companies with strong market positions, brands and corporate cultures. For more information, visit www.sarnova.com
About Digitech
Digitech is a leading provider of advanced billing and technology services to the EMS transport industry. Since its founding in 1984, Digitech has refined its software platform to create a cloud-based billing and business intelligence solution that monitors and automates the entire EMS revenue lifecycle. Digitech leverages its proprietary technology to offer fully outsourced services that maximize collections, protect compliance, and deliver results for clients. For more information, visit https://digitechcomputer.com/
About R1 RCM and R1 EMS
R1 RCM is a leading provider of technology-enabled revenue cycle management services which transform a health system’s revenue cycle performance across settings of care. R1 EMS, formerly known as Intermedix, provides solutions for EMS agencies to help them optimize revenue while promoting superior patient care – from dispatch to discharge. R1 EMS offers comprehensive revenue cycle management services and solutions that provide EMS agencies with billing, coding, collections, dashboards and reporting support. For more information, visit https://www.r1rcm.com/
About Patricia Industries
Patricia Industries, a part of Investor AB, makes control investments in leading companies with strong market positions, brands and corporate cultures within industries positioned for secular growth. Our ambition is to be the sole owner of our companies, together with strong management teams and boards. We invest with an indefinite holding period, and focus on building durable value and capturing organic and non-organic growth opportunities.
About Pamlico Capital
Pamlico Capital is a private equity firm founded in 1988 that invests in lower middle market companies in the U.S. Pamlico Capital seeks control-oriented growth equity investments alongside proven management teams in its target industries: business & technology services, communications, and healthcare. Since inception, the firm, based in Charlotte, NC, has invested over $3 billion. For more information, visit https://www.pamlicocapital.com/
Innovative Technology in the Face of Crisis
As the first line of defense in our communities, EMS personnel need support now more than ever. Agencies and organizations across the country are pooling their resources to help serve and make a positive impact during this crisis.
Sullivan County Emergency Medical Services, the primary EMS provider for Sullivan County, TN, provides aid to about 150,000 citizens and visitors, as well as those in surrounding communities. A number of ambulances and first responder agencies spread across Sullivan County are ready to respond at a moment’s notice, as their mission is to provide “the best emergency and non-emergency care to patients and their families at the worst times in their lives.”

The progressive care provided by the service personnel of Sullivan County EMS (SCEMS) is often described as an “extension of the emergency room,” where the years of experience offered by the County’s personnel of highly-trained Medical Directors, Paramedics, and EMTs allow them to maintain a “continuity of care from the place of origin to the hospital.” Since 1970, it has been their prerogative to have as many trained personnel on scene of an emergency as soon as possible.
In this particular line of work, “seconds count,” and Sullivan County EMS has committed to having the right systems in place in order to lower response times to medical emergencies within their growing communities. Part of their ability to provide such timely service is due to Sullivan County’s tiered response system, which allows for readily-available, localized teams to respond preemptively:
“These response teams bring manpower and multiple levels of training –from Medical Doctors to First Responders– to the crisis environments faced by our Paramedics and EMTs quickly and efficiently. These teams are highly lauded amongst emergency medical personnel for their selfless acts. With their short response times, they have repeatedly induced appropriate care and –most importantly– prolonged viability of life in the field prior to our arrival.” – Gary Mayes, Regional Director
Sullivan County EMS is not alone in providing care and support for their people. In this rural community, EMS is a third service for the County, acting as an extension of the Sullivan County Regional Health Department (SCRHD). The SCRHD also helps to prepare the County for public health emergencies. Their Public Health Emergency Preparedness Department, recognized by NACCHO Project Public Health Ready, uses “an all-hazards approach for emergency planning, focusing on situations that specifically affect the health of the public.” The SCRHD serves the communities of Kingsport, Bristol, Bluff City, and Piney Flats within Sullivan County. Their department’s workforce of around 90 personnel also works closely with the Northeast Tennessee Healthcare Preparedness Coalition in preparing their response to public health emergencies like the one we are experiencing today.
The collaboration between Sullivan County EMS and their Health Department combined with their support from Digitech as an EMS billing partner has inspired inventive measures to combat the COVID crisis. As technological innovation is at Digitech’s core, the evolution and design of new tools in the Ambulance Commander software system ensures that partners will have access to such timely solutions. With data gleaned from Digitech’s recent COVID-19 Symptom Map, Sullivan County has been able to identify the areas within their community in the greatest demand of care. This insight allows them to strategically place future COVID-19 testing sites, so Sullivan can continue to support their most vulnerable populations.
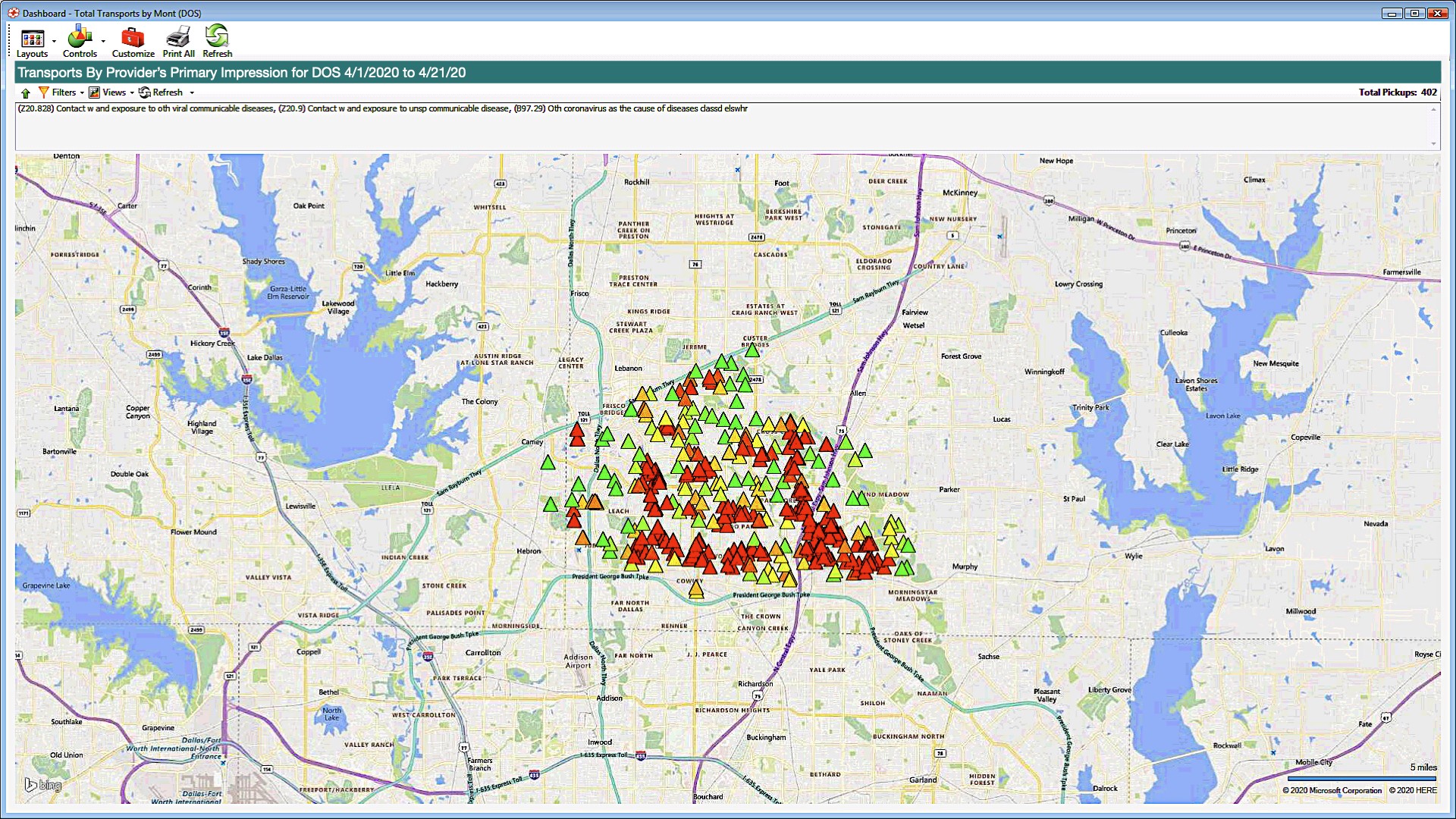
“The COVID Symptom map can be a helpful tool in mitigating the virus by determining specific communities that may need testing, quarantine, or treatment. It allows EMS and Health departments to work collaboratively during the COVID Pandemic.” – Brandon Alley, Sullivan County EMS
The gears continue to turn in Sullivan County as leaders look to this new Ambulance Commander tool for even more creative solutions in the future, like tracking flu-related incidents.
Between these partnerships and updating their Facebook page with information and guidelines on COVID-19, mental health tips, and to thank individuals making donations to support their emergency service providers, Sullivan County EMS continues to commit to their mission of looking out for every single one of their neighbors in need.
Sources:
- Sullivan County EMS, http://www.sullivancountyems.org/main/
- Sullivan County EMS, “First Responders.” January 7, 2015. http://www.sullivancountyems.org/main/section/first-responders
- Sullivan County EMS, “Emergency Services.” January 7, 2015. http://www.sullivancountyems.org/main/section/emergency-services
- Sullivan County Regional Health Department, “History.” 2017. https://www.sullivanhealth.org/about-us/history
- Sullivan County Regional Health Department, “Emergency Preparedness.” 2017. https://www.sullivanhealth.org/emergency-preparedness
- The Northeast Tennessee Healthcare Preparedness Coalition. 2020. http://nethealthcoalition.org/
- Digitech Computer. 2020. https://digitechcomputer.com/.
- Digitech Computer, “New Utilities in Ambulance Commander.” April 24, 2020. https://digitechcomputer.com/new-utilities-in-ambulance-commander/
- Sullivan County Emergency Medical Services Facebook Page https://www.facebook.com/SCEMSOfficial/
New Utilities in Ambulance Commander
Coronavirus Incident Tracking Tools
Our ability to adapt to an ever-changing EMS landscape is a benefit to our clients. We’ve released new tools to help track Coronavirus-related incidents in your service area.
With this latest development, Incident Mapping allows you to:
• Isolate incidents by diagnosis code
• Get a color-coded visual map of your service area’s hotspots
• Interactive maps allow you to drill down to the individual call record
• Adjustable settings to scale heat map coloring based on call volume and service area geography
• Built in integration with Triage utility to display COVID-related pickup locations regardless of provider’s impression
Reach out to your account manager for detailed training by clicking here.
Important COVID News
From all of us at Digitech,
For the duration of this Public Health Emergency, we remain committed to assisting the EMS community by sharing important, up-to-date information with all of our friends and partners. Keeping our clients informed on the most recent updates related to COVID-19 continues to be a top priority. Below is a list of important COVID-19 related industry changes:
- CARES Act Provider Relief Fund – legislation has passed that provides $100 billion in relief funds to healthcare providers on the front lines of the coronavirus response. Due to the importance of delivering the funds expeditiously, the Department of Health and Human Services (HHS) is distributing $30 billion of the relief funds immediately. Please find a summary of the program below. Click here for more details.
- The payments are not loans and will not need to be repaid.
- Payments will automatically be received if your organization received Medicare (FFS) reimbursement in 2019.
- The payments will be received via ACH with a payment description of “HHSPAYMENT”
- Within 30 days of receipt of payment, providers must either accept the payment by signing an attestation and accepting the Terms & Conditions or contact HHS and remit the payment as instructed
- HHS has provided a formula for an estimate of the amount expected which is the amount paid by Medicare in 2019 divided by $484 billion and multiplied by $30 billion. Please contact Digitech if you would like assistance with calculating your estimate.
- The CARES Provider Relief Fund Payment Attestation Portal is now available through hhs.gov/providerrelief.
- Medicare FFS Sequestration Suspension – The CARES Act has temporarily suspended the 2% payment adjustment currently applied to all Medicare FFS claims due to sequestration. The suspension is effective for claims with dates of service from May 1 through December 31, 2020. Providers can expect to receive an increase of 2% more in their Medicare payments during this time period as compared to prior to the suspension.
- Beneficiary Signature Rule Change – Crew members can now obtain a “verbal consent” from the patient to sign on behalf of a suspected or known COVID patient. It is important to note that an actual patient signature is still required in the event the patient is physically or mentally capable of signing and is not a suspected or known COVID patient. Click here for more details, and here for an updated signature form.
- Alternate Destination – CMS has temporarily expanded the list of allowable destinations for ambulance transports to include any destination that is able to provide treatment to the patient in a manner consistent with state and local EMS protocols.
- Accelerated Payment Process – In order to increase cash flow to providers of services impacted by COVID-19, CMS has expanded the current Accelerated and Advance Payment Program to a broader group of Medicare Part A providers and Part B suppliers. The expansion of this program is only for the duration of the public health emergency. It is important to note that these payments are subject to recoupment. Click here for more details.
- CMS Relaxes Physician Certification Statement Signature Requirements – The Centers for Medicare & Medicaid Services (CMS) has released guidance that recognizes the difficulty ambulance service providers and suppliers may have during the COVID-19 Public Health Emergency (PHE) in obtaining a physician certification statement (PCS) signed by a physician or other authorized professional. CMS and its contractors by extension will not deny claims during a future medical audit even if there is no signature for non-emergency ambulance transports, absent an indication of fraud or abuse. Ambulance service providers and suppliers should indicate in the documentation that a signature was not able to be obtained because of COVID-19. The AAA advises completing the PCS form and then indicating if a physician or other appropriate person has not signed it by writing “COVID-19 Public Health Emergency” on the signature line. CMS also reminds providers and suppliers that medical necessity still needs to be met. The full Q&A document can be accessed here.
If you have any questions at this time, please reach out to us.
Digitech Expands Sales Operations with EMS Industry Veterans
New SVP of Sales named to lead business development operations
Chappaqua, NY – February 14th, 2020 – Digitech, a leading provider of EMS billing and technology services, today announced that Jason Crowell has been named Senior Vice President of Sales and Lauren Elam and Scot Metcalf have been brought on as Regional Sales Manager for the Eastern United States and Regional Sales Manager for the Southeastern United States.
Crowell comes aboard from ESO Solutions, where he was Director of Sales for the EMS data company’s EMS, Fire, and Billing Divisions. He brings more than twenty years of experience in business development and sales in the EMS marketplace. As SVP of Sales, Jason will lead expansion into new territories and new markets as Digitech continues to reach for greater opportunities.
“Successful service to the EMS billing community is deeply rooted in trust and financial performance,” says Jason. “Digitech has consistently built trust and delivered results in the marketplace, and because of the reputation they have maintained over their many years of service, I couldn’t be more excited to join this team. I look forward to leading our growth initiatives.”
Elam joins Digitech’s team from Fire Recovery EMS. Her background also includes time as a firefighter and paramedic at City of Bristol Fire Rescue, where she rose to the rank of lieutenant before moving into the private sector. Lauren’s wide range of experience broadens the scope of Digitech’s outreach to Fire and EMS professionals. Metcalf was also a firefighter paramedic at the City of Oviedo Fire Rescue, served as EMS Coordinator for HCA Hospitals, and was most recently Regional Account Manager for ESO Solutions. Scot’s breadth of knowledge in pre-hospital medical services brings a wealth of professional expertise to Digitech’s Sales team.
Digitech looks forward to leveraging the new team members’ experience to guide the company’s next phase of development. “We have an aggressive growth agenda,” states Mark Schiowitz, CEO and President of Digitech, “and we’re confident that Jason is the right pick to lead our Sales team into the next level of engagement with the EMS community. With the support of seasoned professionals like Lauren and Scot, we believe that we will ultimately bring Digitech’s advanced billing technology and premium customer service to a much wider range of ambulance service providers.”
To view this press release as a PDF, please click here.
Where in the World is Digitech – Q1 2020
Tradeshows and Events
Digitech’s road warriors are starting 2020 with a busy schedule full of industry conferences. These events are great opportunities for us to stay at the forefront of the latest trends in EMS and revenue cycle management, and we always look forward to meeting our clients and new contacts on the exhibit hall floor or over a meal after hours. Here’s where you can catch up with us for the first few months of 2020.
Fire-Rescue East
Where: Hilton Daytona Beach Convention Center, Daytona Beach, FL
When: January 22-25, 2020
How to Find Digitech: Exhibit hours are on Thursday, January 23 from noon to 6 PM; Friday, January 24 from 10 AM to 4 PM; and Saturday, January 25 from 9:30 AM to noon. Find us at Booth #1027 in the Exhibit Hall.
TASA Mid-Winter
Where: Park Vista Resort, Gatlinburg, TN
When: February 19-21, 2020
How to Find Digitech: Our team will be exhibiting and mingling in the Park Vista Resort for the duration of the conference. You can find us in the vendors’ exhibit area, or catch us at breakfast or lunch.
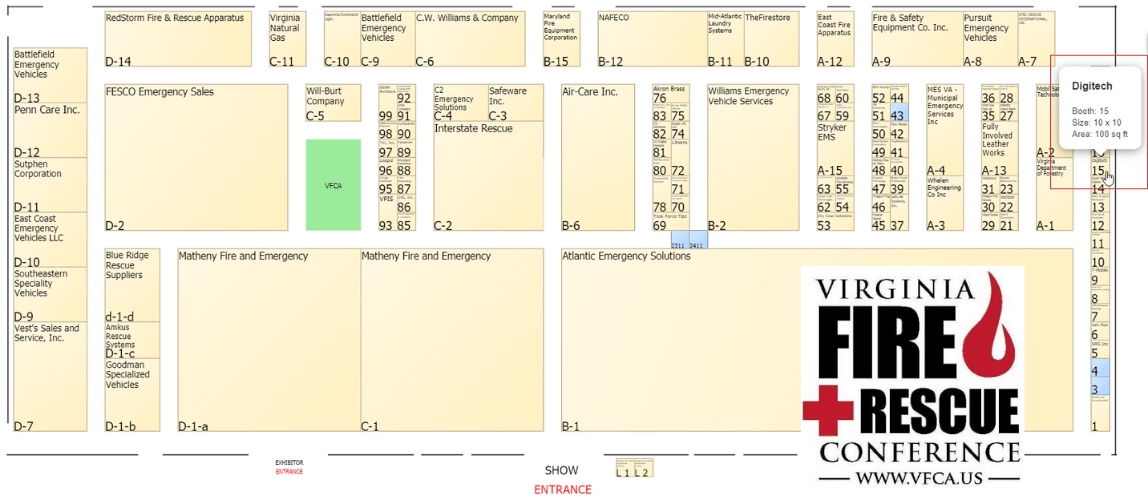
Virginia Fire Rescue Conference
Where: Virginia Beach Convention Center, Virginia Beach, VA
When: February 19-23, 2020
How to Find Digitech: We will be exhibiting on the show floor at Booth #15 during the exhibit hours of 2-6 PM on February 20, 10 AM – 5:30 PM on February 21, and 9 AM – 1 PM on February 22nd.
ESO Wave
Where: Hilton Austin, Austin, TX
When: February 24-27, 2020
How to Find Digitech: We’ll be spending time with our clients and ESO friends during this conference. You’ll see us as both a conference sponsor and an exhibitor at the conference hotel.
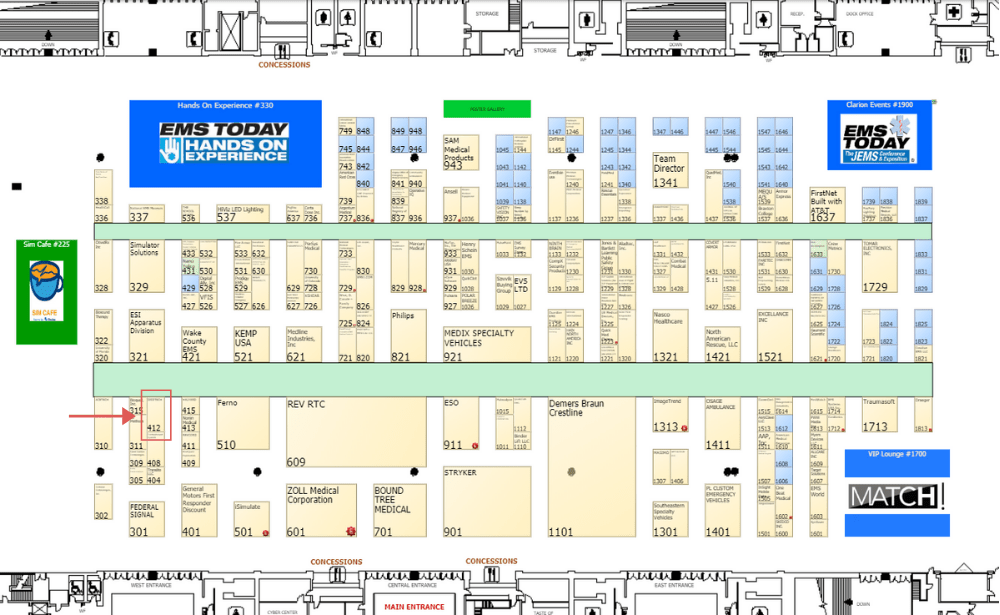
EMS Today
Where: Tampa Convention Center, Tampa, FL
When: March 2-6, 2020
How to Find Digitech: Visit us on the exhibit hall floor at Booth 412. We’re also one of the sponsors for the the $10,000 cash giveaway – good luck!
GEMSA Directors and Leadership
Where: Legacy Lodge & Conference Center at Lake Lanier, Buford, GA
When: March 23-25, 2020
How to Find Digitech: We’ll be at our exhibit booth in the hotel lobby – see you there.
PWW abc360 – Las Vegas
Where: Planet Hollywood Resort, Las Vegas, NV
When: March 22-26, 2020
How to Find Digitech: One of our experts will be speaking at the XI session, and we’ll be at our exhibit booth during the show.
Digitech Receives Investment From Pamlico Capital
Strategic growth investment supports Digitech’s continued success as it enters a new phase of growth
Chappaqua, NY – June 21, 2019 – Pamlico Capital (“Pamlico”) announced that it has entered into an agreement to make a strategic growth investment in Digitech Computer LLC (“Digitech”), a leading provider of Revenue Cycle Management (“RCM”) and technology solutions for Emergency Medical Services (“EMS”) transport providers. Founder and CEO Mark Schiowitz and the Digitech management team will maintain a significant ownership position and continue to manage the growth of the Company with support from Pamlico. Further terms of the transaction were not disclosed.
“This marks a new chapter for Digitech and the next step in evolving the industry’s foremost billing platform dedicated solely to EMS,” said Mark Schiowitz, CEO of Digitech. “Our mission is to deliver a compliant, high-quality EMS billing service that maximizes revenue for clients as a result of our superior technology, integration expertise, and transparent real-time reporting. Our partnership with Pamlico gives us the opportunity to grow our offerings to support the success of our current and future clients.”
Digitech is partnering with Pamlico at an exciting time. The Company has built a large base of devoted customers and is gaining strong market momentum with continued improvements in its proprietary billing software platform and a steadfast commitment to excellent customer service. Digitech helps clients protect compliance, increase collections, and gain greater transparency by focusing on process improvement and automation throughout the entire revenue lifecycle.
“We are incredibly excited to partner with founder Mark Schiowitz and the rest of the management team,” said Art Roselle, Pamlico Partner. “Digitech has built an advanced, EMS-focused RCM platform that delivers best-in-class results for their clients. We look forward to working with the team to increase Digitech’s presence in the EMS industry and continue to innovate on its core offerings.” Pamlico Principal Scott Glass added, “We look for investments where we can work with entrepreneurs as first-time institutional partners, providing capital and strategic advice to help accelerate growth. Digitech represents a compelling growth platform, and we believe there are numerous opportunities to build on its historical success.”
Digitech will maintain its headquarters in Chappaqua, New York.
Digitech was represented by Robert W. Baird & Co. Inc. (financial advisor) and Dentons US LLP (legal advisor). Pamlico was advised by Alston & Bird LLP (legal advisor).
To view this press release as a PDF, please click here.
Digitech Learning Center Goes Live

Pre-hospital patient care documentation training system launches
Chappaqua, NY – April 4, 2019 – Digitech, a leading provider of EMS billing and technology services, announces the opening of the Digitech Learning Center (DLC). The DLC is a new training resource enabling pre-hospital care providers and first responders to deepen their knowledge of a growing array of topics, including a complete, internally-produced documentation compliance course.
The Learning Center’s programs use video-based training followed by quizzes that verify the participants’ knowledge acquisition. Courses are delivered in manageable sections ranging from 90 seconds to 15 minutes. Documenting Excellence, the first training program on the DLC, features eight sections in which all aspects of data collection and documentation of pre-hospital patient care are covered, including operational data, clinical data, history and vital signs, interventions and observations, billing data, and writing complete and compliant narratives.
The DLC’s programs are designed for busy EMTs, firefighters, and paramedics who can do the work at their convenience—on the job, in a coffee shop, at home, or wherever there’s a free moment and good WiFi. Mobile devices and desktop systems all work equally well to consume the training. The coursework is supplemented by an array of resources and references that participants can use to further advance their documentation skills. Onscreen instructors include EMTs and Paramedics from Digitech’s staff, and material for the courses was developed in conjunction with our Certified Ambulance Coders and Quality Assurance experts along with seasoned Emergency Medical Services professionals at Digitech who understand the components and the value of clean, compliant patient care reports.
“We’re excited to offer this new resource to our clients,” said Mark Schiowitz, CEO and President of Digitech. “This medium makes it possible for EMTS to learn on their schedule and for their agencies to benefit from critical training without the huge costs and inconvenience that goes with gathering groups by taking them off the road. It’s quicker, easier, and better than the traditional classroom approach. The testing and scoring system enables EMS managers to track progress and monitor completion of assignments.”
Digitech has provided EMS billing services to clients across the United States since 1994. “We are a technology company, and the Learning Center is a continuation of our tradition of delivering high-quality, high-tech service and support to the EMS and Ambulance community,” adds Walt Pickett, Digitech’s Chief Operating Officer.
To view this press release as a PDF, please click here.
Solving the Deductible Dilemma with Automation
At Digitech, we don’t see problems—we see opportunities. When a client brings us a question or a problem, we turn it into a challenge. How can we develop a solution that will become a benefit to all who we serve? Can we increase efficiency? Can we write new software that eliminates a roadblock? Can we chart a path through the maze that will lead others out of the same trap?
Take the problem of increasing deductibles in healthcare insurance programs. With costs for health insurance pushing a greater portion of the burden onto the patient, it’s naturally gotten harder to collect ambulance billing claims. Some billing companies might shrug and say, “Well, we’re just going to have to live with a reduction in insurance collections and an increase in self pay claims.”
Not here.
At Digitech, we got to work. We’ve rolled out new automation that enables our verification process to check the deductible information on commercial insurance coverage on a case-by-case basis. For those payers that provide this information, it will be captured in the claim record and will allow us to see whether that claim will hit the patient’s deductible. When a significant portion of the bill may get pushed to the patient, we can hold the claim for a period of time to allow for a greater chance for the deductible to be met. This process is in addition to our standard process of holding Medicare and some Medicare HMO claims for deductibles.
The goal here is the one that Digitech always pursues, while keeping a sharp focus on compliance: Maximized revenue for clients and minimum distress for patients.
Going forward, all Digitech clients can opt in to this program. We’re ready for you! Please reach out to your account manager at Digitech to opt in to deductible eligibility checks and we will get the ball rolling for your service.
You may also contact the Digitech team at accountmanagers@digitechcomputer.com.
Ambulance Cost Data Collection Update
The ambulance industry has been abuzz about cost data collection requirements set forth by the Bipartisan Budget Act of 2018. As the system continues to develop, we will provide updates about the timeline, any modifications to the requirements that may arise, and how you can take action. Read on, or download this information as a PDF.
What is the purpose of H.R. 3729, the “Comprehensive Operations, Sustainability and Transport Act of 2017?”
- Medicare Ambulance Add-On Payments, an important supplemental reimbursement source from Medicare, expired on January 1, 2018.
- Congressional action was needed to restore the add-on payments and they were extended with some reductions by the Bipartisan Budget Act of 2018 until December 31, 2022).
- There is a current lack of cost reporting data among suppliers of ground ambulance services.
- This legislation would help CMS understand how much it costs to provide ground ambulance services to Medicare beneficiaries.
- This act would reauthorize the add-on payments for five years as well as create a cost-reporting system that will lead to improvements in the Medicare Ambulance Fee Schedule and adequate payment rates for Medicare transports.
- H.R. 3729 will authorize CMS to design and launch a cost reporting system.
What does the implementation look like?
- Pre-Rulemaking — CMS will engage stakeholders to solicit recommendations.
- Rulemaking — CMS will publish a proposal for collecting cost data then seek public comment.
- Final Rule — CMS will issue a final rule after reviewing public input.
- Launch — CMS will select ambulance services to submit data.
- Phase One — All ambulance service suppliers will provide data on the characteristics of their operation such as the type of supplier (e.g. volunteer rescue squad, private company, third service, etc.).
- Phase Two — A survey will collect cost data from a statistically significant number of each group of supplier and provider to obtain costs and other data.
What will this mean for ambulance service providers who are selected to provide data?
- This is not like Medicaid cost reporting, state reporting, or GEMT reporting.
- Costs for providing services vary greatly due to differing state, local, and agency protocols like bundling.
- Different providers have different fee structures and CMS needs the whole range.
- A representative sampling of providers will be selected to report cost, revenue, utilization, and other information as determined by CMS.
- Data will be collected each year from 2020 through 2024.
- Cost reporting will continue at least every three years from 2025 on.
- Future reimbursement will be dependent on the accuracy and completeness of the data compiled.
How can you take action?
- HR 3729 Bill Tracker
- IAFC Action Center
- Sign up for email updates @ AAA Cost Data Collection Information page
- Sign up for the AAA Webinar series
- Understand what will be required of you and be prepared to collect the required data if your agency is selected
- View the AAA’s report from the 2018 Annual Conference
How can Digitech help you?
If you are selected, Digitech will support you through the cost data collection process by providing relevant revenue data and other resources and tools. Our reporting and data mining systems will ease the delivery of required revenue data for our clients. If you have questions about what this all means and how it may affect you or your service, do not hesitate to reach out to us.
Digitech Sponsors EMS Industry Speaker at Community Paramedicine Conference
Lt. Kevin Spratlin to cover innovations in Memphis Fire EMS response
Chappaqua, NY – May 1, 2018 – Digitech, a leading provider of EMS billing and technology, is proud to announce that the company will be sponsoring Lieutenant Kevin Spratlin of the City of Memphis Fire Department to speak at the Atrium Health 2018 Community Paramedicine Conference. The educational event, held May 7-8 in Charlotte, North Carolina, offers programming aimed at promoting community-based healthcare. Lt. Spratlin is one of a select group of speakers covering topics that support the event’s mission.
Lt. Spratlin’s presentation, “How Memphis Fire Uses Data and Innovation to Navigate Patients to Better Care,” will address the department’s strategy for managing its large non-emergency EMS call volume. Lt. Spratlin leads the Healthcare Navigator program, which includes several initiatives geared toward helping low-acuity patients access the most appropriate healthcare resources. For example, in the City’s RADAR (Rapid Assessment Decision and Redirection) pilot program, for those calls deemed non-emergent by 911 dispatch, a vehicle is sent to the location staffed with a paramedic and a doctor, rather than dispatching an ambulance. The team makes a medical assessment at the scene to determine if emergency care is necessary; if not, they will advise and assist the patient with a different course of action, such as booking an appointment with a primary care doctor or providing transportation to a clinic.
“The results have been encouraging so far,” said Spratlin. “By providing services through the Healthcare Navigator Program, we alleviate the strain on the city’s finite EMS resources, improve throughput in hospital emergency departments, and decrease the cost of care to the healthcare community.” The program involves a collaboration with IBM through the Smarter Cities Challenge initiative, which provides analysis and consultation to reveal patterns in the City’s 911 calls and assess the City program’s effectiveness over time.
Digitech has provided EMS billing services to the City of Memphis Division of Fire Services since 2010. “We are honored to sponsor Lt. Spratlin’s presentation, and we share his priority of allocating the right resources at the right time through innovative, technology-based solutions,” said Mark Schiowitz, President and CEO of Digitech. Several members of the Digitech team will be joining Lt. Spratlin for the Atrium Health Community Paramedicine Conference.
To view this press release as a PDF, please click here.
Same Dashboard. Better Results.
You asked, we delivered.
All New Features on Digitech’s highly acclaimed ![]()
Digitech’s development team has added some cool new features:
- Multi-select Filtering – Drill down on multiple data points at once
- Zooming and Scrolling – Zoom in your horizontal view to better view large numbers of data points
- Legend Quick-Filter – Hide or show data points with a checkbox in the legend
- Cross-hair – Show a vertical cross-hair to make reading line graphs easier
Let us know what you think! Reach out to our Account Managers if you have any questions.
Using Data Analytics to Build Business Acumen
Budgets, reports, revenue cycle management, cash flow, forecasts – there is a mountain of financial data that the modern EMS provider has to track to be an effective organization. What should the Operations Chief or Chief Financial Officer expect from their billing company? Here, we explore the analytical solutions developed by Grady EMS that have helped the 911 service provider for the City of Atlanta to stay ahead of the game.
Presenters:
- Tamara Nilmeier, Director of EMS and Physician Revenue Cycle for Grady Health System, Atlanta, GA
- Michael Colman, VP – EMS Mobile Advanced Practice at Grady Health System
- Mitchel Holder, Executive Director of Analytics at Digitech, former Battalion Chief of Business Services for Gwinnett County Fire and Emergency Services
In-House Billing Is Out of Control
It’s been argued that in-house billing affords ambulance companies more control. You can, after all, walk into your billing manager’s office and ask questions. But don’t confuse proximity with getting the answers and information you need to increase billing productivity. We’re long past the time where geography is meaningful when it comes to data. That’s why companies got rid of their servers — server farms do the job better.
So it is in billing services. Location is irrelevant; concentrated billing expertise and infrastructure are essential. One call to a billing service gets you more help than someone down the hall — even someone with a lot of experience. Reason? An internal billing manager processes 25,000 or 50,000 transports a year while a billing company expert processes a million transports a year for 100 different entities while surrounded by experts in government compliance, insurance industry regulations, and Information Technology. Where are you more likely to get the best information?
You could say control is your access to information that is critical to your decision-making, in which case you have less control than you think. You have some flexibility, assuming you have someone in-house who has some skill with running reports, or you pay the software vendor to produce the reports. Compare that with a billing service with proprietary software and a comprehensive and customizable reporting system. The billing service has an analytics team of IT pros and industry specialists who can produce any report you can imagine for little or no cost. They’ve also gone up the learning curve, so you don’t have to. In fact, they may have already solved your problem because they’ve worked on it with other clients.
Or perhaps your definition of control is the ability for management to make changes to the billing process or personnel as needed. That’s a bit more difficult to tackle. When does the owner of an ambulance company realize she needs to make a process or personnel adjustment? Probably when cash flow is crippled or an audit reveals errors that entail a sizable pay back – in other words, when it’s too late. And when the decision has been made that change is required, how does that get done? Do you now dig into the billing process, hope you can understand it better than the current manager, and then implement the change yourself? Or do you replace the billing manager? If so, where does that new manager come from? It’s not as if experts in ambulance billing with strong management skills are on every street corner. And what of the people in that department that might be loyal to the old manager?
While we’re on the subject of change, let’s assume you can sense the financial benefit of a software change. You know in your bones that you can save $40,000 a year in payroll if Utility X can be developed or modified. Who do you think is more likely to deliver that development? Hint: probably not your software vendor. They avoid software modifications like the plague because every change made for you has to be transferred to 100 other clients. The vendor also knows that every now and then a client will be lost because they hate a change so much. Billing services are built for change because continuous improvement is a basic component of their proprietary software. They understand they will likely benefit from change because it will also make their job easier.
Maybe control is the ability to have an external auditor conduct an audit at will. Engaging an industry expert to audit a claim sample is pretty easy if you have the budget. Realistically, ambulance company owners rarely do, because it’s distracting, it’s time consuming, and it may test morale. Billing services, on the other hand, do these things as a matter of course and will often send you summaries of the reports. They thoroughly understand the process in that they probably go through more audits in a year than most ambulance companies go through in a lifetime. They have a verifiable track record. And you have control in knowing you can push the audit button at any time, even if you rarely do. 
Ultimately, control is about the ability to make changes seamlessly whenever circumstances dictate change is necessary. The ultimate control is being able to replace a billing service without causing too much disruption. You simply start talking to other billing services, give them some data, and ask them to show you how they can solve whatever problems you have and provide better solutions. The conversion process may be a bit stressful, but it is manageable — assuming the service has a decent transition process. That part you can verify from references.
It may seem odd to suggest that billing services are interchangeable parts. They’re not. Some are better than others. But being able to replace them quickly gives the ambulance company operator the ultimate control: You’re never stuck with an underperformer.
How Ambulance Billing Services Can Increase Revenue and Maximize Compliance
What business are you in? The answer may seem obvious to an ambulance service manager: “I’m in the emergency medical transport game.” But if you’re also doing the billing for those transports, you’re in fact in two businesses, because emergency transport and medical transport billing are completely different enterprises. It’s a critical distinction with lots of bottom line implications says, Mark Schiowitz, president and CEO of Digitech, who discussed the issue with JEMS during EMS Today 2017 in Salt Lake City.
Agencies that see billing merely as the paperwork portion of transportation can run into costly challenges related to everything from personnel to hardware. Never mind collecting data, how about processing it? “They have to deal with a whole IT infrastructure, which would include security and firewalls, and they need IT people to manage all these servers that they have,” Schiowitz said. “Once they get through that, they have to deal with application software that they need to maintain and keep updated; they need training. And then once they get all that stuff down, they need a whole billing department.”
Agencies that choose to handle their own billing will, of course, need to hire people with highly specialized skills. Good luck finding them. “This is a pretty niche industry; you can’t just find someone who does medical billing and expect them to do ambulance billing,” Schiowitz said. “You need to find some very special people.”
That’s in part because those people have to be fluent in the languages of legal considerations, frequent Medicare updates, medical transport protocols, HIPAA laws, and other security issues. “You have to make sure that your people are trained in compliance. There’s a lot of work, time, and money that goes into setting up a billing department,” Schiowitz said.
Seeking Outside Help
At a minimum some EMS agencies will consider outsourcing to avoid dealing with the increasing IT and hardware requirements. “Most billing companies, at least the good ones, will host the application. Some will even provide a dispatch system,” Schiowitz said. “So you’ve really simplified your infrastructure and, in doing that, you’ve released a certain amount of corporate energy to do the things that your company does best.”
But slimming the infrastructure is just the beginning of how outsourcing billing may help ambulance agencies thrive. How about fattening the revenues and lowering costs? “You have a real possibility that the billing service is going to increase revenue,” Schiowitz said. “You could also reduce your payroll, which creates a much leaner company that is better able to deal with the other issues of your business.”
Schiowitz says that it’s important to keep in mind that outsourcing is a variable cost, one that is linked to revenues as opposed to a monthly subscription that has to be paid whatever the volume. This helps make billing a manageable expense rather than a potentially costly exposure.
Still, many agencies remain resistant to the idea of third-party outsourcing. Sometimes it’s a friend or family member who’s doing the billing or, as is frequently the case, the agency genuinely believes it can do as good a job as a specialty billing service. The risk for the agency is that it’s extremely difficult to be good at both. The ambulance agency’s prime focus has to be on providing quality patient care and meeting response times. That raises the likelihood that it won’t be as good at disciplines such as compliance. Billing companies are solely focused on billing and all the regulations that come with it. “We have to be, because our whole company is at risk,” Schiowitz said. “If we run [afoul of] a compliance issue, clients will leave us, so we are extremely focused on compliance.”
Pitfalls
As with any investment, you have to conduct due diligence before outsourcing your agency’s billing. “You really need to be sure you’re picking an entity that can increase collections, has the compliance record, and has the track record to achieve the results that you want,” Schiowitz said. “And the second thing you need to do is you need to be committed to the project. Some companies will try to keep two or three of their billers on staff to manage the billing company. That’s a little bit like telling a doctor how to cure you. You really need to commit to the billing company and accept the fact that they probably know how to do this better and let them take the lead.”
EMS and ambulance agencies should be cautious of investing in a billing software system rather than a full-service billing solution. “A company that’s selling software is not incentivized to maximize collections or maximize efficiency,” Schiowitz said. “You’ll have companies that are selling by the seat, for instance. The more seats they sell, the more money they make and the more support fees they get, so they’re not inclined to reduce the numbers of seats they sell. There’s no incentive for a third-party vendor to try to help an ambulance company maximize revenue.”
In contrast, a full-service billing company is specifically designed to maximize revenue and efficiency. “The difference is that theirs [the software company] might be a Cadillac. It’s comfortable, easy to use, anybody can drive it,” Schiowitz said. “But what you really need is speed – something closer to a Formula One.” Never mind the air conditioning, the music system, or other accessories, says Schiowitz. “Focus on performance. Forget about the five-passenger comfort and just have a system that is specifically designed to achieve superlative results, which includes maximizing revenue, maintaining compliance, and delivering deep and transparent reporting.”
The Dirty Secret Your Software Vendor Won’t Tell You
Companies that sell billing software to the ambulance industry never fail to promise that their software will increase efficiency and profits. What they haven’t mentioned is that their software improves their efficiency and profits, not yours. To achieve that, they sell software that is inferior by design. There. We said it.
To be fair, they have no choice. Software companies can’t make money selling billing software to the ambulance industry – at least not real money as defined by the technology industry. So they have to sell low performance products to maintain their bottom line. How can this be, you ask?
Let’s say a software company somehow captures the entire New York City non-emergency medical transportation market, one of the largest non-emergency medical transportation markets, at approximately one million transports per year. Say that software company wins a killer deal by charging ambulance companies $2 per transport to use their software (about four times the current market rate). Ultimately, after snagging an impossible share of the market and charging an outrageous rate, the software company generates $2,000,000 in annual revenue – less than the annual revenue generated by the average McDonald’s franchise. Consider that for a second: a software company dedicated to the ambulance industry can’t survive by dominating the largest market on the planet and overcharging.
Given this limited revenue potential, the software companies can only afford to build mediocre, fairly generic products, and they can’t afford to market them as anything less than cutting edge. These vendors will point to their software’s well-organized process flow – but that’s exactly the flaw in the argument. In this system, claims are moved from bucket to bucket within measurable time frames. The system just has to keep track of the claim, and all the biller has to do is manually move the claim from one bucket to the next. How’s that for automation? It’s not particularly efficient, but the software provider benefits because the client needs more seat licenses to keep the volume of claims moving. The software system stays simple and cheaper to maintain, which improves the software company’s profits.
A software manufacturer will similarly avoid adding features that maximize collections because those features require additional system complexity, which increases development costs and complicates implementation, training, and maintenance. In other words, it’s a loss for them to help you collect more.
Here’s the good news: Given that the billing software sold to this industry is weak, at best, there is a significant opportunity to improve collections and efficiency with the right technology and the right partner. You need a vendor whose goals are in line with yours.
The only entity incentivized to develop the technology that will maximize efficiency and collections is a billing service that lives for the challenge of continuously evolving new solutions – because really, they’re the only ones who can afford to. They know that the more automated the process, the more code is required, which increases development and maintenance costs. But they also know that extra development expenses result in improved labor efficiencies, allowing fewer people to handle more claims, collect more dollars per claim, and collect on a higher percentage of claims.
Effective billing companies improve by analyzing exceptions, not ignoring them. When enough similar exceptions are found, the truly efficient billing company is able to build a new automated process flow to capture and properly handle those claims. This kind of company sees agencies’ problems as opportunities instead of obstacles, which creates a rewarding partnership.
So if you accept the notion that technology is the key to maximizing efficiency and collections, the answer should be clear: You need a complete billing service with proprietary software.
Risky Business: The Collection Percentage Guarantee
If you’re a government agency that is going to issue an RFP for ambulance bill collection, demanding a collection percentage guarantee may seem like a good idea. And in some ways, it is: a guarantee requires little thought as to how to develop a better, mutually beneficial partnership with a vendor. While the guarantee is a defined benefit for the agency, it is a risky proposition at best for ambulance billing companies.
Agencies include a collection percentage guarantee in their RFPs thinking that it translates to a guaranteed amount of revenue. Seems logical – if the billing company agrees to a certain benchmark, it has an extra incentive to collect as much as possible, right?
Wrong. For the billing company, this requirement may have the opposite effect.
One way to increase revenue for an agency is a recommendation to raise ambulance fees. While this will likely increase revenue, it may also decrease the collection percentage. Let’s say a billing company collects 100% of a $400 claim. If the agency increases its rate to $1,000 and the billing company now collects only 50%, they increase collections by $100 but cut the collection percentage in half. This is an extreme example, but it makes the point: If a billing company is expected to maintain a minimum percentage or be penalized, it is actually being discouraged from doing everything it can to maximize collections.
The billing company then has two choices: Ignore the risk of reducing revenue by focusing on the collection percentage, or face penalties for not holding up its end of the deal. This assumes, of course, that the billing company doesn’t put the agency at risk by up-coding claims – billing a level of service higher than what is medically necessary, or showing all adjustments as contractuals – to meet the agreed upon percentage.
A collection percentage requirement will scare off some bidders who could otherwise handle the job well. Reason? The vendors most willing to risk the penalties of underperforming are those who have the legal resources to fight those same penalties. Are you hiring a billing service or a law firm? Or are you looking for a company that collects the minimum for the maximum profit without looking to become a true consulting partner? In either case, your agency could be unknowingly cheating itself out of superior service.
Any way you slice it, a required collection percentage guarantee is a certainty that the vendor/client relationship becomes either a little bit dishonest or not mutually beneficial. If your goal is to maximize revenue with the help of a trusted partner, steer clear of percentage guarantees. Any company willing to enter into such an agreement does not have your best interests at heart.
Finding Money Ain’t Cheap
Should your ambulance billing service collect $16 million in billings for you or $20 million? Seems like a stupid question. But what if the service knows they will make a profit of $240,000 on the $16 million but only $140,000 on the $20 million?
It’s more expensive to process claims that involve denials, appeals, and multiple phone calls. If your billing service collects an average of $250 per transport and charges 5% of collections, they make $12.50 per claim. What are they supposed to do with claims that need a $20-an-hour-employee to stay on the phone for an hour? Some billing services will ignore these claims; it’s more profitable to write them off and send them to the collections graveyard. And if you’re the EMS client, it’s your agency that loses, not the billing service.
Perhaps you are thinking your billing service has an ethical obligation to work every claim, and if you agreed to pay a set fee per claim, they clearly do. But when the fee structure is an incentive-based percent of collections, things get a bit murky. When paying a percent of collections, you’re basically telling your billing service, “We want you incentivized such that the more money we make, the more money you make – and if we make no money, neither do you.” If that’s the case, is it really a violation of the deal for the billing service to choose not to make money for you on the claims that are not profitable for them?
Everyone in government and business is looking for the best price. EMS chiefs and finance officers have to consider the lowest-price option when seeking bids for goods and services. That’s not only logical, it’s the law in many cases. But low cost and cost effective are not the same thing. Every good manager knows this. Yet when purchasing decisions face the scrutiny of an elected board of commissioners or a finance director or a purchasing office, managers need to have a strong justification for not buying the cheapest available product. Municipalities need to keep two things in mind: First, the profit-oriented private sector does not think like the politically accountable public sector; second, it’s really difficult to beat people at their own game.
For manufacturers and service providers, lowering the price has a number of ramifications, not all of which are pleasant. On the plus side, a low price:
- Forces efficiencies
- Makes a business clarify what’s essential
- Fosters competition
But there are negatives too, including:
- Forces cost cuts that affect training, support, and the quality of life you can provide to your employees
- Quality gets compromised
- The safety and security of your people, your PHI, and your investments may suffer
Any seller can cut price, but great brands offer something beyond low price – convenience, dependability, service, or innovation, for instance. Consider Jet Blue in the airline industry or Amazon in retailing. In the world of EMS billing, that “something beyond” is the ability to process every claim profitably while charging a competitive fee. Few ambulance billers can do that.
The math of collections is worth doing. You may be able to realize double digit collection increases with a single digit fee increase. The higher fee will cover the costs of the technology and advanced processes that can increase collections far beyond the difference you may be paying out. While initially more expensive, applying advanced technology to pursue every dollar on every claim will produce a substantial amount of incremental revenue.
Fire chiefs, revenue cycle managers, finance directors, and municipal officials need to consider their options carefully when making decisions about which billing company offers the best value for their organization. You might think you’re getting a bargain with a billing service that offers a low cost per claim, but just because something is cheaper doesn’t mean it’s a better value. When you’re paying people to find you money, don’t be surprised if they find more when you pay more.
The Right Partner
 Every growing business is faced with critical, make-or-buy decisions. Accounting, tax, customer service, office management, maintenance — at some point these functions suck up too much time and resources to be handled internally. They distract you from your company’s main task: delivering a valued service to customers.
Every growing business is faced with critical, make-or-buy decisions. Accounting, tax, customer service, office management, maintenance — at some point these functions suck up too much time and resources to be handled internally. They distract you from your company’s main task: delivering a valued service to customers.
That’s especially true for billing: Outsourcing your billing with the right partner will outperform in-house billing every time. That partner will collect more, cost less, maintain a higher level of compliance, and often provide better reporting and analysis.
Why? Because the right partner’s collection software is better than your collection software — even if you’re buying from a third-party software “specialist.” You’d like to think that buying from a third-party vendor will give you the best-performing software available. But that’s not the case. In fact, using a third party vendor can almost guarantee that you won’t have best-in-class collections. That might seem contradictory. After all, wouldn’t a software specialist strive to provide the best product out there? The answer is no. The specialist’s business model doesn’t work that way.
A company that bills in-house must do two things to maximize profit: 1) collect everything it’s entitled to; 2) be as efficient as possible – that is, minimize the number of billers in the department. To try to accomplish that, the firm purchases billing software from among the small group of vendors that specialize in ambulance billing software.
This is where the economics get interesting, and not necessarily in a good way. The third party software companies are similarly striving to maximize profitability, which turns the vendor-client relationship into a zero-sum game. That means the more you get, the less they get — and vice-versa. Some partnership. To enhance their own profitability, software companies have an incentive to minimize the efficiency of their own product and pay less attention to helping clients maximize collections.
And therein lies the rub that has cost ambulance companies millions over the years. The contemporary software model is to sell by the seat license. The more seats a software vendor sells, the more revenue it earns and the higher its long-term (forever) monthly support fee. That system has worked pretty well for Microsoft, a company never accused of being customer-centric. If a billing software company boosts efficiency, it will sell fewer seats. Even worse, increasing the software’s efficiency also increases its complexity, which in turn raises costs for development, implementation, training, and support. Overall, that’s a really bad deal for the software company — inflating costs to reduce revenue has never been a good long-term business strategy.
Somewhat perversely, the software company is similarly incentivized to resist helping its client improve collections. To improve collections requires developing and testing new modules, upgrading a working system, re-training billers, and adding support costs. As firms rarely like to upgrade their software, even less so if they have to pay for it, the upgrade cycle becomes difficult. And if conscience, competition, and pride force the vendor forward (damn those torpedoes), losing a client for making that effort will likely recalibrate the conscience instantly.
Why would you lose a client for doing good, you might ask? Change creates frustration at the client’s company, wherein the software company has to deal with the ire that comes with upending the daily routine of billers who benefit naught from the improved collections. That sometimes leads to complaints to the owner who, aware of his complete dependence on his billing manager, may utter something like, “If you don’t like our vendor, go find one you do like.” SURPRISE! The billing manager likes the one that doesn’t need or require continuous upgrades.
The solution is to find the “right” billing partner, meaning not just any billing partner. You’ll need to do a bit of digging. Take a look under the hood. Develop a set of requirements. The good news is that choosing is less subjective than you might think as it revolves around the technology in use – or rather, that technology’s origin.
For starters, any billing service that uses someone else’s technology is in the same position as the entity that bills in-house. In fact, this partner could underperform the in-house group because it’s savvy enough to know which claims are profitable to collect and which aren’t and may decide to focus on those that are profitable. It’s classic Low-Hanging Fruit Syndrome. If they use someone else’s software, remove them from your list.
Identifying the right partner begins with the right technology. You’ll recognize it if they own their own processing software and have made a long-term commitment to improving its efficiency and ability to maximize collections. You’ll know this is the case if:
- They have a staff of full-time programmers who work exclusively on this software. It’s a bonus if those programmers have a ton of experience with the company.
- They upgrade their software regularly (weekly) and every client receives the benefit of those upgrades.
- They can point to specific modules they have released in the last year that have improved collections or efficiency or both.
- They offer full transparency. In other words, the service allows the client to access the billing system 24/7, produce a list of claims on screen that represent every transport done for a specific date range, and enables the client to drill down into each claim and find out everything that was done to collect that claim.
Those capabilities are a healthy start. You’ll know you have a partner who shares your priorities and has committed resources to achieve them. And you’ll know you have a partner that does not fear transparency. They won’t be trying to hide anything.
But there’s more you can do. If your partner has large municipal clients, you’ll know it has the following qualifications as these are required by many municipalities:
- The firm has a solid IT infrastructure with good Disaster Recovery systems.
- The firm has been audited by independent external auditing firms that are experts in the field.
- The firm has audited, publicly available financial statements.
- The firm has SOC 1 Audit results, which are reports by external auditor who insure this company meets its contractual obligations.
- HIPAA and PHI breach data is publicly available.
References should be at the heart of any evaluation. While there are many companies that do ambulance billing, there are only a few that do it on a large scale. And in most cases, clients have moved from one of these top-tier companies to the other. Ask potential vendors to speak to clients that they have taken from competitors and then ask the clients about the circumstances under which they left. Who collected more, who responded better, how did their implementations compare, whose reporting was better? If one company’s name keeps popping up, and that company meets the criteria above, then maybe you’ve found the right partner.
Apples and Oranges: The Problem with Comparing Collection Percentages
In completing over 500 responses to RFPs over the past 10 years, Digitech has encountered the requirement of a collection percentage guarantee multiple times. The municipality’s goal in including this requirement, we suspect, is to identify the agency with the higher collection percentage because that agency will collect more money. While intuitively this may seem inevitable, in reality and where medical billing is concerned, it is not.
Experience has shown us that collection rates for ambulance transports are dependent on several factors: the payer mix and demographics of the area, the speed of claims processing, the agency’s rates, treat-no-transport billing or not, and a number of other inputs that are variable across different types of agencies and different geographic locations. What applies to one emergency transport provider may not apply to the next. Even with reasonably accurate carrier mix data, using collection percentages as a means of comparing billing companies can be misleading. Comparing one service’s collection rate to another’s is often a futile attempt to make the apple taste like the orange.
Given the relationship between actual collections and collection percentages, a collection percentage guarantee is often not advantageous to the provider agency. Think about it: Would you prefer a vendor that collects 100% of a $400 charge or 50% of a $1000 charge? Increasing collections often means suggesting that you bill higher ambulance fees that will generate more revenue and, in the process, lower collection percentages.
On average, Digitech collects approximately 99% of the Medicare and Medicaid allowed amounts, between 80% and 93% of insurance, and anywhere from 1% to 8% of private pay. The overall collection percentage depends on the client’s payer mix. For instance, if all claims were Medicare claims, Digitech’s overall collection percentage would be 99%. If the payer mix is comprised completely of private pay claims, our collection percentage would be 8% or below. These are obviously extreme examples, but they illustrate the impact of carrier mix on overall collection percentage.
So if collection percentage analysis is not the best way to compare vendors, what is the alternative? We recommend looking at collections per transport (CPT) because it is generally a clearer measure of collections as it removes variance due to volume. This makes it easier to compare vendors’ performance. Ask the billing companies you’re considering for examples of where they have taken over from other companies and compare CPT. Then call those entities and ask specific questions.
Another way is to look at the technology that each prospective billing company is using and dig into its capabilities. Superior technology is the most significant determinant of success in ambulance billing. The best companies will have mature, well-conceived, customizable software that is specifically designed for ambulance billing.
Finally, references should be at the heart of any evaluation. In many cases, clients have gone from one billing company to another. Ask the clients about the circumstances under which they left their previous vendor. Who collected more? Who responded better? How did their implementations compare? Whose reporting was better? Answers to these questions paint a much more complete picture of prospective companies than collection percentages will.
Collection Improvement Examples
Digitech has increased revenue recovery for our clients every time we have been contracted. Click on “Before” and “Digitech Year 1” to see how much.
Houston Ambulance Chase Nets $28 Million
Supplemental payment program closes the gaps in reimbursement for ambulance transports
Briarcliff Manor, NY – December 11, 2015 – When the Houston City Council selected Digitech to handle its billing for ambulance transports in 2013, it signed on with a partner that could help the city address both an information gap and a budget gap. A federal program allows governmental ambulance providers to recover a portion of the difference between the actual cost of services provided and the reimbursement allowed under Medicaid, Medicaid Managed Care, and uninsured patients. Houston had been missing out on these Ambulance Supplemental Payment Program (ASPP) funds, because it couldn’t be certain of providing the extensive documentation of these expenditures required by the state of Texas, which administers the program.
Digitech’s Ambulance Commander software, combined with their data mining experience and reporting expertise, enabled Houston to provide the detailed accounting of all the city’s ambulance trips required by the ASPP. Houston had already seen an $11 million increase in revenue captured from ambulance billing—from $29 million in 2012-13 to nearly $40 million in 2013-14. For 2013-14, the ASPP has returned almost $28 million in additional revenue to the City of Houston. Digitech projects a similar return for Houston for the 2014-15 fiscal year, which will help the city close a projected $63 million budget gap. “The City Council made a wise decision in Digitech,” states Mayor Annise Parker. “Their direction and support in recovering revenue from the Ambulance Supplemental Payment Program has brought a big payoff for Houston.”
“These results are outstanding,” adds Digitech CEO Mark Schiowitz. “We knew there was the potential for a substantial return from the ASPP, and we knew we could deliver it.” Digitech’s deep specialization in ambulance billing protocols has gained national attention for improving collections in several major municipalities. The company’s detailed reporting and conscientious approach to compliance continue to lead the way to increased revenue for ambulance service providers.
To view this press release as a PDF, please click here.
Case Study: Digitech Goes Live in Four Weeks at Gwinnett Fire and EMS
Adapted from a Digitech implementation study – full PDF available for view or download here.
Rapid expansion means increased call for services
Gwinnett County, a suburban community of the Metro Atlanta area, has seen rapid population expansion accompanied by increased demand for services. The Gwinnett County Department of Fire and Emergency Services, formed in 1997, has since expanded as well. Maintaining a dependable revenue source to meet the Department’s rising operating costs became imperative.
Gwinnett issues call for proposals
By 2011, Gwinnett County had identified medical transport billing as a revenue source that might benefit from improved efficiencies. The Department was already using ESO Solutions ePCR software on Panasonic Toughbooks to generate electronic patient care reports from the field, which had brought improvements to the accuracy and completeness of their field data collection. Gwinnett was also using a bank lockbox for direct deposit of remittances to streamline the posting of receipts. Now the need was to speed up submissions – to be able to pull the data from the field reports, review claims and add information if necessary, submit claims to third party providers and receive remittances, all within a shorter time cycle. After extensive research into best practices and in-service solutions deployed at similar departments around the region and nationally, Gwinnett County assembled and issued an RFP for emergency medical billing services. The opportunity was right in the sweet spot for Digitech, who excels in creating process efficiencies for medical transport billing. Digitech knew they would submit a proposal.
Digitech sees opportunity
“The contract was something we really wanted to pursue as the County is considered a trend setter in the region,” reported Marty McNellis, Director of Business Development for Digitech. “We felt our robust reporting capability would be well received by the Gwinnett Fire Rescue, who were hungry for data and able to make good use of it.”
Digitech’s Ambulance Commander, the proprietary software platform which McNellis describes as “the heart and soul of Digitech’s ability to file claims” has been 25 years in development. “It’s already been integrated with all of the major ePCR applications,” said McNellis, “and has numerous customizable features that enable the Digitech development team to adapt it easily to the particular requirements of any implementation project.” Most importantly, Ambulance Commander’s track record is very solid, and has proven to increase collections with a high degree of success.
Implementation begins
The contract was signed in late November and systems integration began immediately. “This was a fairly smooth transition,” commented Walt Pickett, Digitech’s Senior VP Development and support. “We had a great team to work with on their side – very well organized.” However, Digitech’s implementation was required to meet the benchmarks of the contract, one of which was a January 1 start date. Fortunately, because Digitech had already implemented an interface between the ESO Solutions ePCR software and Ambulance Commander, the deployment team was able to shortcut that piece of integration. The Gwinnett implementation of Ambulance Commander was made operational within four weeks, ready for the “go live” date planned for end of December. At the same time, Digitech account managers were preparing enrollments with third party insurance carriers such as Medicare and Medicaid at the same time they were gathering authorizations for the electronic transfer of remittances. “The credentialing process requires several steps,” reported Mary DelFranco, Digitech’s Senior Account Manager. “By posting payment in this way, it becomes much more efficient compared to keying data in manually.”
Also within this four week period, Joyce Kerulo, Digitech’s Senior VP for Billing Services, and her staff were getting prepared by setting up an organizational structure to handle the account. “One of our strengths is that we are able to process quickly,” she said, “usually within one business day of receiving claims.” Donna Buhler, CPA and Business Manager for the Gwinnett County Fire and Emergency Services Department, agrees. “Joyce always responded immediately to any of our change orders,” she stated. “She and the Digitech Billing team were always very thorough in everything they did.” As the first ESO ePCR reports were being received from Gwinnett County during the last week in December, Digitech staff began verifying third party insurance information using Digitech’s proprietary search process, Sleuth. Trained coders looked for the compliance issues to ensure third party insurers were being billed for the correct level of service. The first submissions were made to Medicare and Medicaid on January 6th, 2012. Within a window of some 14 days, Gwinnett County began to see remittances deposited into their lockbox account. Digitech’s Director of Finance reported that average monthly receipts between March and August 2012 totaled $1.3 million. 17% of that total was achieved during the first month of operation – January, 2012, and 77% during the second month. By the third month – March, 2012, Gwinnett County was receiving 100% of the $1.3 million average total and has maintained that amount in monthly remittances ever since.
Digitech follows through
“They exceeded our expectations in the way they were able to implement,” said Department Chief Mitch Holder, Battalion Chief, Business Services. “Any time we addressed an issue they were very proactive in delivering solutions, usually within 24 to 48 hours.” Once Digitech had demonstrated it could continue to deliver services as specified in the contract over a significant stretch of time, it was a good moment to cement the relationship with a face-to-face meeting that could help the County to take their reporting, their processes, and their planning to new levels.
“The transparency of Ambulance Commander’s reporting systems allows us to troubleshoot on any issue and about anything,” Chief Holder now says, commenting on the software. “The dashboard is a useful tool. We use it to create financial reports, or to research the age demographics of our patients, or to identify insurance carriers. We’ve seen a change both in the type of patient we transport and an increase in the number of transports. The software enables us to project future needs and build that into our budget process.” Donna Buhler agrees. “The reporting capabilities are extensive and accessible,” she says. “I can pull up any information that I need or drill down to any detail of any individual transport. My monthly reconciliation process is much less of a challenge and goes more smoothly.”
To continue reading the full case study, please click here to view the PDF.
Digitech Compliance Officer Receives National Certification
Silverman among the first in the nation recognized under new designation
Briarcliff Manor, NY – October 21, 2014 – Digitech Computer, Inc., a leading provider of hosted billing services for ambulance transport agencies, announced today that Jane Silverman, the company’s Chief Compliance Officer, has received certification from the National Academy of Ambulance Coders as a Certified Ambulance Compliance Officer. Ms. Silverman is among the first class of Compliance Officers to be certified under the new designation.
The Patient Protection and Affordable Care Act of 2010 (Obamacare) has brought legal and regulatory compliance front and center for ambulance transport agencies, and the institution of the new CACO program is one way that NAAC is responding to the challenge. Under the PPACA, agencies, institutions, and municipalities that receive reimbursement from Medicare and Medicaid and other federal healthcare programs are subject to new requirements and regulations around the handling of chronically ill or “Frequent Flyer” patients, new cost containment mandates, and new quality standards for pre-hospital care. The law established Accountable Care Organizations to monitor and control reimbursements for healthcare providers, while also monitoring the quality of care delivered to patients. PPACA also sets up a Medicare Shared Services Program (MSSP), which allows the ACOs to contract directly with Medicare. Providers, including EMS services, that wish to reap the benefits of Accountable Care Organizations will need to examine their processes and procedures carefully in order to maintain compliance.
Having a Certified Ambulance Compliance Officer on your side can provide a tremendous benefit to clients attempting to negotiate this changing healthcare reimbursement landscape. “The CACO training I received has been incredibly valuable to the development of a state of the art, highly professional compliance program at our organization,” states Ms. Silverman. “The depth and breadth of the material presented, along with the strong support of the management team at Digitech, ensures that we have a compliance culture based on solid legal and ethical principles.”
“That culture of compliance will be extended to Digitech’s clients,” adds Mark Schiowitz, President and CEO of Digitech. “We believe it’s our responsibility as a partner to make sure that our clients are engaged, informed, and actively invested in their own compliance programs.”
To view this press release as a PDF, please click here.
Digitech Wins Product Innovation Award
PCR Lens earns EMS World award
Briarcliff Manor, NY – December 2, 2013 – EMS World magazine, a publication of Cygnus Business Media and voice for the EMS community, has named PCR Lens from Digitech the winner of a 2013 Product Innovations Award. EMS World’s Top Innovation Award Program recognizes companies that have produced new and original products to serve EMS providers, enhance pre-hospital patient care, or deliver better solutions to meet new requirements and emerging market needs. PCR Lens, included with Digitech’s EMS billing service, is a tool for EMS administrators and leaders that provides a means to measure and improve field data collection.
EMS providers find themselves increasingly challenged to capture patient information, document procedures and medications, and write accurate narratives that will support reimbursement and compliance. As private and government insurance providers have become more stringent in their requirements for the documentation of patient care during ambulance transports, the need to deliver complete and accurate patient care reports has become more and more important.
“PCR Lens aggregates the pre-hospital data from each run as it comes across through the Patient Care Report application and puts it into an interactive user interface,” states Walt Pickett II, SVP of Implementation and Support for Digitech. “PCR Lens can then display the data in a variety of user-defined views, making it easy for EMS leaders to zero in on problems, push training and re-education to where it’s needed, and identify high performance individuals and crews.”
“We are pleased that Cygnus has honored our efforts to create a product that serves the Quality Improvement needs of EMS providers” says Mark Schiowitz, Digitech’s CEO and President, “at the same time it helps improve collections for EMS Billing claims. Better data translates into better collections, and that’s a win-win situation.”
“Product Innovation Awards for software have been rare, because most innovations in EMS come in the form of tools and delivery systems for patient care,” said Nancy Perry, Executive Editor for EMS World, “but Digitech’s PCR Lens fills a need that will continue to increase in importance as agencies institute more quality controls in response to tighter regulation of billing for emergency transports.”
To view this press release as a PDF, please click here.
Digitech Projects Major Collections Improvement for Baltimore
Baltimore City sees immediate improvement with new EMS Billing vendor
Briarcliff Manor, NY – September 30, 2013 – Digitech Computer, Inc. today announced that collections for emergency transports under its contract with the Baltimore City Fire Department have outstripped projections by more than 50%. Based on current run rates, Digitech will collect several million dollars more from 2013 EMS transports than were collected in 2010, the most recent year for which data from fully resolved claims processed by the previous vendor is available. Collections per claim have climbed from $108 per claim in 2010 to a projected $160 per claim in 2013. Digitech began processing claims for Baltimore in December, 2012.
All municipalities that run EMS operations are entitled to reimbursement for their services from insurance companies, state or federal governments or individuals. But payment is highly dependent on accurate data and claims processing. “The increase in collections is the result of some courageous decisions made by Baltimore officials,” says Mark Schiowitz, CEO of Digitech. “Working with the outstanding leadership of BCFD, we were able to apply Digitech’s industry‐leading technology to deliver vastly improved results at a time when every dollar counts for budget‐constrained cities.”
The Digitech team, working with Baltimore City Fire Chief Alex Perricone, (Deputy Chief of EMS), Chief of Fiscal Services Jim Fischer, and Chief of Staff Steve Nutting drew up a set of recommendations to increase the city’s EMS transport collections rate, which lagged behind the national average.
—First, the team developed an intensive training program to improve the quality of documentation of patient care by Baltimore EMTs. Deployed in combination with Digitech’s PCR Lens tools, better documentation enabled Baltimore Fire to significantly improve the accuracy of field data collection, which in turn creates cleaner claims with fewer denials and appeals.
—Second, the team improved accuracy in transferring field data to the billing system, resulting in an immediate 32% increase in the
number of billable claims.
—Third, Baltimore officials established data exchanges with local hospitals that enabled Digitech to download patient insurance and
demographic information directly into the claims creation process.
—Finally, the Committee deployed a new inventory system for data collection equipment to ensure that EMTs always have updated,
working devices—you can’t process data that you can’t collect.
These procedural and policy improvements, in combination with Digitech’s leading‐edge reporting tools, have enabled Baltimore City
Fire to generate an up‐to the‐second accurate picture of EMS operations and stay on top of the department’s finances.
“With Digitech’s help, we’ve brought our EMS billing into the 21st Century,” says Jim Fischer. “It took some pushing, and change is never easy, but the results speak for themselves.”
To view this press release as a PDF, please click here.
Plano Renews Digitech Contract
City exercises option to extend EMS billing agreement
Briarcliff Manor, NY – July 29, 2013 – Digitech Computer, Inc. announced today the City of Plano, Texas, has extended their contract for EMS Billing and Collections for another year, exercising their option to renew the original 2‐year deal signed in July 2011.
Assistant Chief Jim Dickerson heads up the Emergency Operations Division of Plano Fire‐Rescue and is responsible for the delivery of a range of emergency and non‐emergency services to the Plano community. “Digitech was the right choice for EMS billing for Plano,” states Dickerson. “They combine a technology‐driven approach to ambulance billing with a strong commitment to customer support. It’s been a great partnership.”
Digitech initially came on board to handle EMS billing for Plano in 2011 after the City had completed an exhaustive study of the EMS service operating within the Plano Fire Department. The report made it evident that a top‐tier billing company was required to help Plano Fire‐Rescue address the challenges they faced. Accuracy in billing, thorough followup, and a comprehensive electronic process for filing medical transport claims were clearly called for. Plano’s department is regarded as a national leader by fire administrators, so the opportunity created an opening to make a strong impression in the Texas fire community. Digitech was pleased to step up to the challenge, and the result has been very favorable. “Digitech is as committed to us now as they were in the beginning, and they are as
professional and prompt to respond,” says Sonora Copling, Senior Administrative Assistant for EMS and Training for the city of Plano. “No matter who I speak with, I am treated as if there is no other place that person would rather be than on the phone helping me. I can think of no bigger compliment.”
Walt Pickett, II, SVP of Development and Support for Digitech, says, “The folks at Plano have been really sharp right from the start – asking the right questions, understanding what they needed to do, taking advantage of the tools and services we’ve provided to them – they made my job much easier.”
To view this press release as a PDF, please click here.
Greenbrier County Goes Live with Digitech
EMS Billing Service Implementation a Success
Briarcliff Manor, NY – July 15, 2013 – Digitech Computer, Inc. announced today the successful implementation of EMS billing services for Greenbrier County Emergency Ambulance Service. GCEAS, based in Lewisburg, West Virginia, is a major provider of emergency medical care and ambulance transports in Southeast West Virginia. Greenbrier County marks the first client for Digitech in the state of West Virginia.
“The project came off without a major hitch,” said Walt Pickett, II, SVP of Deployment and Support for Digitech. “We got Greenbrier up and running in just under 60 days from contract signing to the go-live date.”
The speedy implementation is a testament to the years of effort that Mr. Pickett and his team of developers and account managers have directed towards creating an efficient plan for delivering a project of this scale. The Greenbrier deployment provided an opportunity for the team to test the new platform that Digitech has developed to manage new client implementations. The platform, called Pedestal, assigns and tracks every task that is part of implementing a hosted EMS billing service. Those activities include the filing of all necessary payer registration paperwork, the creation of all business rules and patient communications required for a new client, setting up secure links between systems, software customization, and tracking claim status end-to-end. All are required elements to enable an EMS billing company to create and invoice the claims for ambulance transports carried out by the client.
“We’ve found the right EMS billing partner in Digitech,” stated Jerry Kyle, Administrator for Greenbrier County Emergency Ambulance Service. “They have made the on-boarding process very easy for us, and have guided us through every step. Walt and the entire Digitech team have proven themselves to be very professional and very supportive. We look forward to the fulfillment of the business relationship we’ve launched here.”
To view this press release as a PDF, please click here.
Digitech Undertakes Massive IT Upgrade
Firm gears up to gain speed, reliability, and scalability
Briarcliff Manor, NY – April 9, 2013 – Digitech Computer, Inc. announced today the completion of a large‐scale project to upgrade and improve the company’s Information Technology architecture and systems, marking the culmination of a complex mission to redesign and rebuild its communications and data warehousing infrastructure with virtually no interruption to existing business processes.
Digitech has grown organically for over 28 years, but several factors converged to make this the right time for a major leap forward. Dramatic reductions in the price of hardware, new software that enables near immediate recovery from any hardware failure, and the ability of the .NET release of Ambulance Commander to take advantage of the latest hardware combine to improve reporting and maximize collections for Digitech’s Ambulance Billing clients.
“While we’ve always been able to sustain growth without sacrificing the instant availability of systems and information that our clients rely upon,” states Ben Lambert, Digitech’s VP of Technology. “We knew that continued growth would require us to upgrade backup systems, remove unnecessary complexity in our IT architecture, optimize hardware utilization, and eliminate potential vulnerabilities. We’ve now moved to a virtualized setup that enables us to add excess capacity whenever we need it with no delays and no downtime.”
Digitech undertook vigorous investigation of current best practices in IT, bringing in consultants and specialists to guide research and validate network designs. Server clusters with failover systems optimized at every point of the communications infrastructure now provide security and reliability that will anchor many years of future growth while eliminating vulnerabilities, trimming access points, and reducing the amount of actual hardware that’s at play in the system by almost 70%. “Our large in‐house development team combined with the increased stability of our systems will enhance our speed to market with new integrations, upgrades, and process changes,” says Walt Pickett II, Digitech’s SVP of Implementation and Support. “We’re ready to serve our clients better and faster.”
“We’re solid as a rock,” replies Mark Schiowitz, Digitech’s CEO and President, adding, “We always say that technology is in our DNA – now we’re stretching our technological lead. We have no key man vulnerability, no vulnerable piece of hardware or equipment, and all systems and processes are now completely hardware‐agnostic.”
To view this press release as a PDF, please click here.
Digitech Readies EMS Data Quality Reports
PCR Lens creates visibility into EMS operations
Briarcliff Manor, NY – February 25, 2013 – Digitech Computer, Inc. announced today the release of PCR Lens, the latest reporting module for its flagship Ambulance Commander® EMS Billing and Dispatch system. PCR Lens will provide EMS administrators, medical directors, crew chiefs, and business analysts a 360° view of operational effectiveness from the standpoint of field data collection. The system presents an opportunity to collate and analyze field data through a straightforward and intuitive user interface.
As private and government insurance providers have become progressively more stringent in their requirements for the documentation of patient care during ambulance runs, EMS providers have found themselves increasingly challenged to capture patient information, document procedures and medications, and come up with accurate narratives to support reimbursement of transport claims. A single piece of missing information is often the difference between billable and unbillable claims.
“PCR Lens aggregates the prehospital data from each run as it comes across through the Patient Care Report application and puts it into an interactive user interface,” states Walt Pickett II, SVP of Implementation and Support for Digitech. “Ambulance Commander can then display the data in a variety of user-defined views, making it easy for EMS leaders to zero in on problems, push training and e-education to where it’s needed, and identify high performance individuals and crews.”
“We designed this tool to give administrators the ability to compare how well medics are collecting data, how their data aggregation kills compare to other techs in the department, and how the entire organization’s data aggregation skills compare to other unicipalities across the country,” says Mark Schiowitz, Digitech’s CEO and President. He added, “These reports make it possible to identify weaknesses in the data collection process, develop responses to correct those weaknesses, and measure improvement. The end result is a more compliant system and better collections.
“We’re all aware of the need for good data, but we’re piling up mountains of information that we’re not making good use of,” said Kurt Steward, Assistant Director at Dallas Fire Rescue, who was part of the beta test of PCR Lens. “Digitech has provided an extremely useful set of tools to make sense of that data. We are excited to see how we can make use of the data moving forward as part of our Quality Improvement Program.”
To view this press release as a PDF, please click here.